Approximate Read Time: 13 minutes
“Pain is a messenger. The real skill is learning when to listen, when to respond with topical pain relief, and when to let biology do its work.”
What You Will Learn
- How topical formulations interact with skin, circulation, and pain pathways.
- Which ingredients are proven vs placebo in sports-related muscle pain.
- How to apply and how to decide what works for you or your athletes.
The Athlete’s Paradox
Athletes live in a paradox: we chase adaptation through discomfort, but we spend careers trying to control pain. The pain relief area at the local pharmacy is crowded — cooling gels, CBD balms, menthol sprays, “anti-inflammatory” patches promising to erase soreness overnight.
The reality? Only a handful of topical agents consistently deliver clinically meaningful relief. Most others live somewhere between mild efficacy and placebo.
I’ve experimented with a variety of lotions, gels, and patches. My goal here isn’t to sell magic creams — it’s to separate mechanism from marketing, bring us back to key principles, and to show you how to use topical therapies within a structured rehab and recovery model.

Why Topical Matters
Pain relief is usually divided into systemic (pills, injections) and local (topical, physical, manual). For athletes, local therapy makes intuitive sense: apply the medicine where it hurts.
Unlike oral NSAIDs, topical formulations deliver high concentrations directly to subcutaneous tissue with minimal systemic absorption, reducing gastrointestinal and renal side-effects (Stanos, 2007). That’s why many sports medicine clinicians prefer gels and patches during in-season phases when oral medications can interfere with recovery or hydration.

But skin absorption isn’t automatic. The skin’s stratum corneum — the outer layer of skin cells — is both the gatekeeper and the barrier. Molecules and particle size matter in order to be able to bypass certain layers of the skin efficiently (Stanos, 2007). That’s why diclofenac, ketoprofen, and lidocaine — small molecules — consistently show therapeutic tissue levels without systemic toxicity (Derry et al., 2016).
The Science of Pain: A Quick Primer
Pain is a conversation between damaged tissue, the peripheral nervous system, and the brain. Nociceptors (sensory nerve endings) respond to mechanical, thermal, or chemical stress. They transmit impulses via A-delta and C-fibers to the spinal cord and, eventually, to higher centers where the sensation becomes “pain.”
Topical analgesics work primarily by interrupting this signal — either at the source (reducing inflammation and prostaglandin production) or along the nerve.
In sports medicine, two categories of topical analgesics dominate this space:
- Pharmacologic topicals — NSAIDs, local anesthetics, counter-irritants.
- Natural / naturopathic topicals — herbal and cannabinoid-based compounds.
Each targets different parts of the pain pathway.
Topical NSAIDs: The Gold Standard
Topical NSAIDs are the most evidence-backed option for athletic pain management. Diclofenac and ketoprofen lead the category, with meta-analyses showing significant pain reduction for acute strains and chronic overuse injuries (Derry et al., 2016; Shi et al., 2023).
In the Cochrane review of 10,857 participants, 60 percent of those treated with topical diclofenac experienced ≥50 percent pain relief versus 50 percent for placebo with minimal side effects (Derry et al., 2016). Ketoprofen gel performed slightly better.
What matters clinically is how they compare to oral NSAIDs. Systemic absorption from topicals is typically under 5 percent, yet functional outcomes for conditions like tendinopathy, DOMS, and mild osteoarthritis are similar to oral routes (Stanos, 2007).
For athletes, that means you can manage localized inflammation without compromising renal function, gut health, or blood pressure — a valuable advantage during heavy training blocks or multi-day tournaments.
How They Work
Think of NSAIDs, like a diclofenac patch, as peacekeepers sent to quiet an inflamed neighborhood. Inside that neighborhood, two troubled teenagers — enzymes called COX-1 and COX-2 — keep churning out chemical “fire alarms” known as prostaglandins. These alarms call in swelling, heat, and pain. When an NSAID steps in, it temporarily silences those teenagers, turning down the volume on the body’s inflammatory response.
When applied to the skin, the medication doesn’t go wandering through the whole city (your bloodstream). Instead, it settles right where the noise started — the dermis and muscle underneath — within just a few hours (Stanos, 2007). It’s like delivering calm directly to the street corner in trouble, quieting the local commotion without disturbing the rest of the body’s rhythm.
Common Drugs
- Diclofenac gel (1–2%) — great for joint and muscle pain; demonstrated efficacy in sprains, DOMS, and knee osteoarthritis (Derry et al., 2016).
- Ketoprofen gel (2.5–5%) — faster absorption; some studies show superior cartilage diffusion (Stanos, 2007).
- Etofenamate gel — less common in the U.S., but may have greater tissue bioavailability (Marinho & Pereira, 2020).
For practical use, I have the most experience with diclofenac as prescribed from the team physicians I have worked with in the past. The physicians often recommended athletes apply a thin layer 2–3 times daily over the affected region with gentle massage to enhance microcirculation. The mechanical rubbing adds a mild gate-control effect by stimulating A-beta fibers that compete with pain signals in the spinal cord.
Lidocaine
Lidocaine patches and creams work like noise-canceling headphones for irritated nerves. Under normal circumstances, nerves send clean, rhythmic electrical signals—like a well-tuned orchestra. But after an injury, some of those nerves start misfiring, sending static and distortion down the line. These misfires, called ectopic discharges, are what create that burning, electric ache athletes often feel around scar tissue or surgical sites.
Lidocaine steps in by blocking the sodium channels—tiny gates that nerves use to transmit their electrical signals (Casale et al., 2017). By closing those gates temporarily, the patch quiets the unwanted noise, restoring calm to the system. It doesn’t numb everything; it simply tells the overactive instruments to take a break so the body can play in tune again.

Unlike oral analgesics, lidocaine acts locally without performance impairment. Athletes can train with patches on for up to 12 hours, though I recommend removing them before sweat-intensive sessions to avoid adhesive slippage.
Counter-Irritants: Menthol, Camphor, Capsaicin
These creams and gels don’t actually fix the injury—they simply distract the nervous system from it. Think of them as a clever magician who draws your attention to one hand while the other is doing the trick.
When you apply something that feels icy cold or warmly tingly, your skin’s sensory receptors light up and send those sensations racing to your spinal cord. Because only so many messages can fit through the same “doorway” at once, these competing sensations crowd out some of the pain signals. That doorway is what scientists call the gate, and when it’s filled with other sensations, pain messages have a harder time getting through.
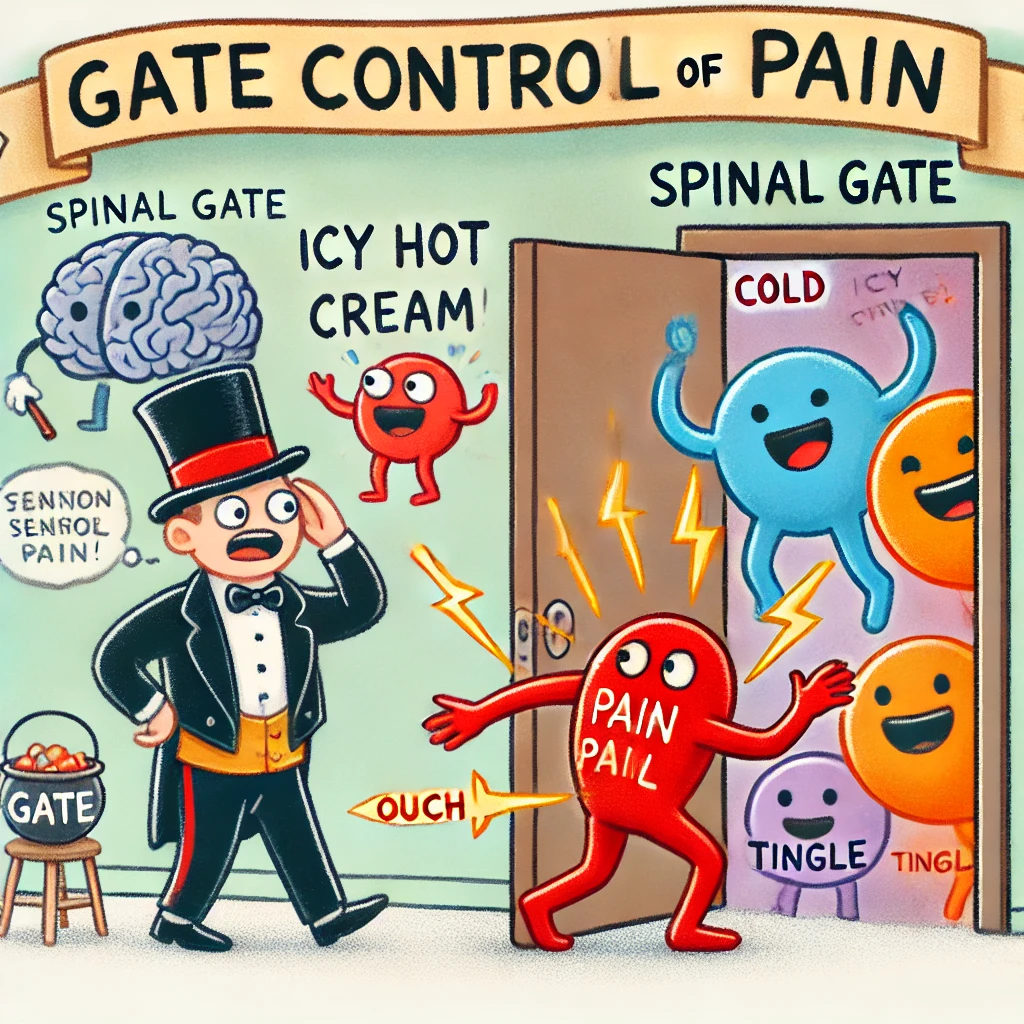
Menthol and camphor are the classic gatekeepers. They create that fresh coolness or gentle warmth that tricks the brain into perceiving comfort. The extra blood flow they bring to the skin can also help wash away some of the metabolic waste that contributes to soreness after hard training.
Capsaicin—the compound that gives chili peppers their heat—works differently. It’s like a short, intense training drill for your pain nerves. At first, it fires them up, creating a fiery sensation. But after repeated exposure, those nerves tire out and stop shouting so loudly. In the clinic, high-dose capsaicin patches can quiet nerve pain by 30–50% (Casale et al., 2017). For most athletes, though, the lower-strength versions are enough to warm the area and take the edge off without feeling like you’ve rubbed on hot sauce.
For everyday use, capsaicin’s lower concentrations in over-the-counter creams can be valuable for chronic joint or tendon pain — but educate athletes to wash hands thoroughly and avoid eyes.
Natural Topicals: CBD, Arnica, and Beyond
The rise of “natural recovery” in sport has brought CBD, arnica, and herbal topicals into training rooms and locker rooms. These products occupy a gray zone—scientifically intriguing, but inconsistently regulated and variably effective. Still, their mechanisms overlap surprisingly well with traditional pharmacology.
CBD (Cannabidiol)
CBD works like a communication coach for the body’s built-in “calm system,” called the endocannabinoid system. Picture this system as a network of cell phone towers spread across your body — in your nerves, skin, and immune cells — constantly sending and receiving signals to keep things balanced. When pain or inflammation jam the lines with static, CBD helps clear up the signal so messages of calm can get through.
It does this in a few ways: it quiets inflammation, dials down overly sensitive pain sensors, and boosts your body’s natural feel-good signals — all of which help you handle discomfort a bit better.
When applied to the skin, CBD doesn’t have to travel through the digestive system — it goes straight to the neighborhood that needs attention. While animal studies show encouraging signs of reduced inflammation, we’re still waiting for stronger human evidence to confirm how well it works.
From my experience, CBD topicals make a good supporting player — not the star. They can help athletes who feel a lingering buzz of soreness or nerve irritation that doesn’t quite respond to traditional options. But like any supplement, quality is everything: I only trust verified products with lab-tested ingredients. A cheap CBD cream with little active compound is like a phone tower with no power — it looks the part, but it won’t send a clear signal.
Arnica montana
Arnica has been a go-to remedy for bumps and bruises for centuries. The yellow mountain flower behind those gels and creams contains natural compounds that help calm swelling and irritation. Think of it as nature’s version of an ice pack in plant form — gentle, soothing, and easy to tolerate.
Research on arnica is mixed. In one study comparing arnica gel with ibuprofen gel for hand arthritis, both eased pain about the same after three weeks, though ibuprofen worked a bit faster (Rondanelli et al., 2020). Arnica’s biggest strength is that it’s mild and generally well-tolerated, making it a good option for easing post-workout soreness or minor bruising.
For athletes, I see arnica as a recovery amplifier — something that helps the body settle down after training. It can boost local blood flow and reduce discoloration from bruises, but it’s not strong enough to replace medical-grade anti-inflammatories when there’s a significant injury.
Essential Oils and Herbal Blends
Blends made with camphor, eucalyptus, menthol, or wintergreen (the familiar scent of “sports rubs”) work by creating a gentle distraction for your nervous system. The cooling or warming sensation they produce competes with pain signals, giving your brain something else to focus on. Beyond that, the smells themselves can encourage relaxation — part science, part ritual.
Research shows these essential oil mixes can provide mild, short-term relief for sore muscles, especially when combined with massage or recovery routines (Bakó et al., 2023).
The Skin Barrier: What Actually Gets Through
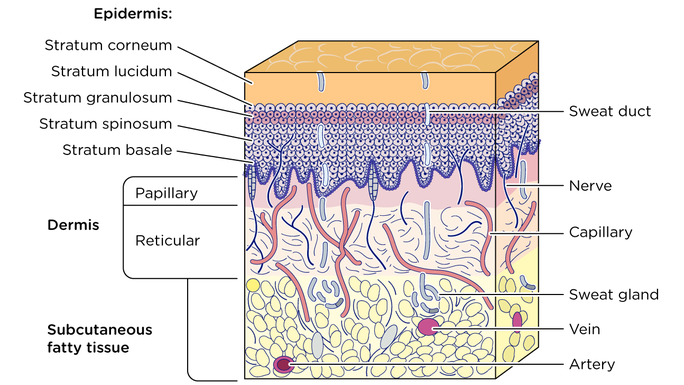
Many topical products fail not because they lack active ingredients but because they can’t cross the stratum corneum, a superficial layer of the skin. Absorption depends on molecular size and the topical product’s ability to hydrate the skin or disrupt lipid layers.
Modern delivery systems have improved absorption dramatically. Gels tend to be better than creams because of the water content within the gels.
Massage and heat increase skin uptake by boosting microcirculation. This is why applying a topical post-shower or after light aerobic work often improves efficacy.
The Placebo Effect: More Than Psychology
Placebo isn’t failure—it’s physiology. When athletes believe a topical will help, the brain releases endogenous opioids and dopamine that reduce pain perception. In long-duration studies of topical NSAIDs, up to half of the placebo group reported substantial pain relief (Derry et al., 2016).
This reinforces a point I teach in mentorship: The ritual matters. Application, scent, expectation—all contribute to the neurochemical environment of healing. Dismissing placebo misses an opportunity.
How I Guide Athletes to Use Topicals
I categorize topicals by intent rather than ingredient:
- Anti-inflammatory – Diclofenac, CBD, Arnica
- Neuromodulatory – Lidocaine, Capsaicin, Menthol
- Circulatory / Recovery – Essential oils, Massage balms, Heat gels
Here are simple guidelines for everyday use:
- Apply to clean, dry skin
- Massage lightly for 30 seconds to stimulate circulation
- Avoid combining multiple agents with overlapping actions (e.g., capsaicin + menthol)
- Patch test first—athletes with eczema or sensitive skin often react to salicylates and fragrances.
- Educate that pain reduction ≠ readiness; use topicals as adjuncts, not replacements for load management.

Where Topicals Fit in the Rehab Continuum
Topicals are tools, not solutions. They serve best in the early and middle phases of rehab to modulate pain, promote movement, and build athlete confidence. In late-stage return to play, systemic adaptation—strength, speed, load tolerance—drives the outcome.
I often describe their role as “quieting the noise” so we can train what matters.
The 3P Model—Principles, Process, and Plans—anchors how I integrate topical pain relief within rehab and performance therapy. It’s not about which cream you use; it’s about how and why you use it. Here are 4 ways we can tie in topical agents with the 3P Model:
- Coordinate Movement
Pain changes movement. A topical that decreases pain enables cleaner motor patterns. If a knee feels “pinchy” a diclofenac gel might reduce guarding enough to restore proper mechanics during a split squat. - Force Management
Topicals can’t generate force, but they can reduce inhibitory signaling that limits it. A lidocaine patch over an irritated hamstring tendon can facilitate early isometrics when eccentric loading still provokes pain. - Fitness and Recovery
Pain relief enhances adherence. Athletes who feel better train more consistently, leading to faster aerobic and muscular recovery. A post-lift arnica or CBD balm supports the recovery. - Treat the Person, Not the Diagnosis
Two athletes with identical imaging may respond differently to the same topical. Individual preference, skin type, and pain psychology all matter.
Summary: Pain Relief Without Performance Compromise
Topical therapies allow us to manage discomfort while respecting the body’s natural adaptation process. Diclofenac and ketoprofen remain the most validated pharmacologic options; lidocaine and capsaicin target nerve-driven pain; CBD and arnica bridge the gap between modern science and natural options.
No topical replaces the fundamentals: load management, nutrition, and recovery consistency. But when used within a structured 3P approach, they reduce friction in the rehab process.
Five Keys to Topical Pain Relief in Sport
- Science over sensation: Cooling doesn’t equal healing.
- Topicals modulate, not cure: They create opportunity for movement.
- Consistency compounds results: Apply regularly, not reactively.
- Quality matters: Look for pharmaceutical-grade, evidence-backed ingredients.
- Integrate within complete rehab plan: topical agents are a tool, not a solution.
Free Download
Read More Like This
Related Podcasts
References
Derry S, Conaghan P, Da Silva JAP, Wiffen PJ, Moore RA. Topical NSAIDs for chronic musculoskeletal pain in adults.Cochrane Database Syst Rev. 2016;(4):CD007400.
Casale R, Symeonidou Z, Bartolo M. Topical treatments for localized neuropathic pain. Curr Pain Headache Rep. 2017;21(15):1–9.
Stanos SP. Topical agents for the management of musculoskeletal pain. J Pain Symptom Manage. 2007;33(3):342–355.
Shi C, et al. Multidisciplinary Guidelines for Rational Use of Topical NSAIDs. J Clin Med. 2023;12:1544.
Bakó E, et al. Efficacy of Topical Essential Oils in Musculoskeletal Disorders. Pharmaceuticals. 2023;16(20144).
Rondanelli M, et al. Clinical trials on pain-lowering effect of ginger and arnica. Phytother Res. 2020;34:2843–2856.
Roy L, et al. Efficacy and onset of Bonipar, a topical analgesic for musculoskeletal pain. Complement Ther Clin Pract. 2024;57:101908.
Picotti S, et al. Clinical investigation of a new hyaluronic acid-peptide topical lotion. BMC Musculoskelet Disord. 2023;24:6903.
Marinho O, Pereira A. Efficacy of topical etofenamate in musculoskeletal disorders. Pain Ther. 2020;9:393–410.
Hohenauer E, et al. Effect of post-exercise cryotherapy on recovery characteristics. PLoS One. 2015;10:e0139028.
Wang Y, et al. Heat and cold therapy reduce pain in delayed-onset muscle soreness. Phys Ther Sport. 2021;48:177–187.
Nitecka-Buchta A, et al. Transdermal cannabidiol for myorelaxation in TMD. J Clin Med. 2019;8(11):1886.
Haroutiunian S, Drennan D, Lipman A. Topical NSAID therapy for musculoskeletal pain. Pain Med. 2010;11(4):535–549.
Dakić M, et al. Effects of massage therapy on sport and exercise performance. Sports. 2023;11(6):101–115.
Dupuy O, et al. Evidence-based recovery techniques to reduce muscle soreness. Front Physiol. 2018;9:403.





