Approximate Read Time: 10 minutes
“Swelling is not the enemy. It’s biology’s signal to heal. The challenge lies in managing it without interrupting the body’s own repair process.”
What You Will Learn
- Why swelling is biology’s signal, not the problem.
- How compression, movement, and devices improve circulation.
- Practical strategies for safe swelling management after injury.
The Evolution of Injury Care
Few acronyms in sports medicine have been as enduring, or as controversial as RICE. In 1978, Dr. Gabe Mirkin coined the term “Rest, Ice, Compression, and Elevation” as the gold standard for acute injury care. For decades, coaches, physical therapists, and athletes alike turned to RICE as the unquestioned blueprint. Ice bags were strapped on everything from ankle sprains to post-game soreness, while athletes were told to “stay off it” until swelling subsided.
But science evolves. Over time, cracks appeared in the RICE framework. Clinical evidence suggested that rest might prolong recovery, and that icing—while great for numbing pain—did little to accelerate tissue healing.
Newer frameworks such as PRICE (Protection, Rest, Ice, Compression, Elevation) and, more recently, PEACE & LOVE (Protection, Elevation, Avoid anti-inflammatories, Compression, Education & Load, Optimism, Vascularization, Exercise) emerged to update our approach to injury management (Dubois & Esculier, 2020).
The debate over ice isn’t just semantics. It represents a fundamental shift in philosophy. Are we treating swelling as a problem to suppress, or as a biological signal to manage?

The Inflammatory Response: Biology’s Repair Kit
To understand swelling, we must first understand inflammation. Injury initiates a cascade that is part biology, part defense strategy.
The arterial system delivers oxygen and nutrients, powered by the heart’s pump. The venous system returns blood toward the heart, but unlike arteries, veins lack strong pumps; they depend heavily on muscle contractions to move blood uphill against gravity.
Finally, the lymphatic system clears excess fluid and metabolic waste. Unlike the arterial & venous system, the lymphatic system lacks a centralized pump. They rely almost entirely on movement, pressure gradients, and tissue contractions to drive flow (van den Bekerom et al., 2012).
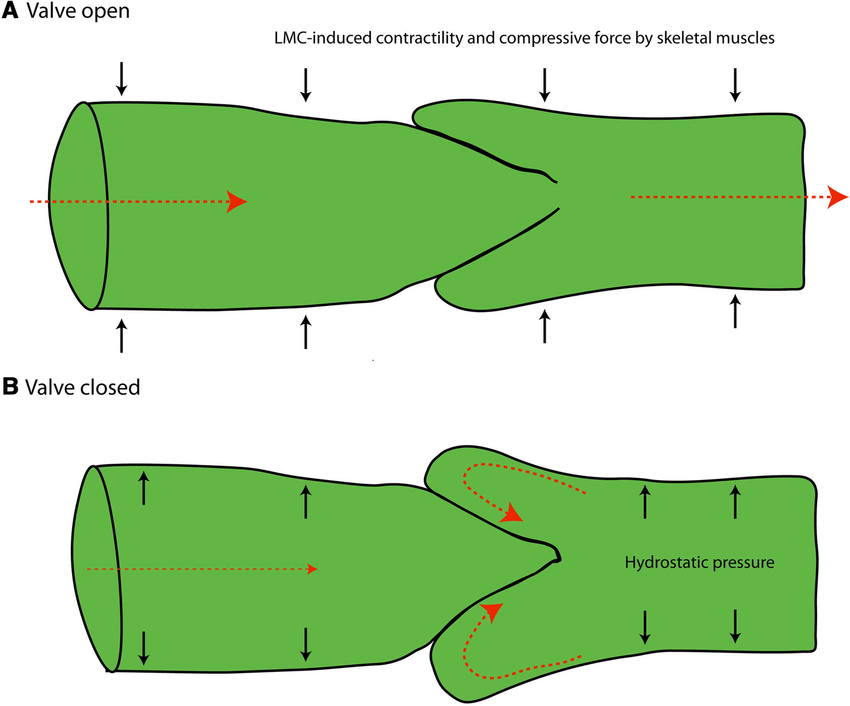
This is why swelling tends to pool in extremities and why immobility compounds the problem. Without contraction, fluid stagnates.
Pain, in this context, is not just a symptom. As Butler and Moseley describe in Explain Pain, pain is part of the body’s “danger alarm system” that is an orchestra of chemical signals, neural activity, and contextual interpretation (Butler & Moseley, 2003). The inflammatory “soup” of histamine, prostaglandins, and cytokines triggers nociceptors (pain receptors), increasing sensitivity to protect the injured area.
In short: swelling is a purposeful biological response. It delivers immune cells, builds scaffolding for tissue repair, and heightens awareness to protect the area. But unchecked, it can limit mobility, increase pain, and delay functional restoration.
FREE DOWNLOAD
Start Optimizing Your Stem Cell Recovery Today with this Recovery Guide!
What Ice Really Does (and Doesn’t Do)
For generations, ice has been the universal go-to. Its primary benefit is clear: pain relief. Cooling tissues slows nerve conduction velocity, numbs sensation, and provides an analgesic effect (Bleakley et al., 2010; Allan et al., 2022).
But pain relief and swelling reduction are not the same.
Cryotherapy can temporarily reduce local blood flow, but studies show its long-term impact on swelling and recovery is limited. A systematic review of ankle sprain management found little evidence that icing accelerates healing or return to play (van den Bekerom et al., 2012).
“Ice is best understood as a pain manager, not a swelling reducer.”
A historical perspective reinforces this point. In one randomized trial, patients with ankle trauma experienced only modest reductions in swelling from continuous cryotherapy compared to more dynamic methods (Stöckle et al., 1997). Similarly, a comparison of cold, heat, and contrast baths found that cold produced the least edema, but none of the methods dramatically reduced swelling over three days (Côté et al., 1988).
The bottom line: ice is excellent for pain control, but not a silver bullet for swelling.
Compression and Pascal’s Law
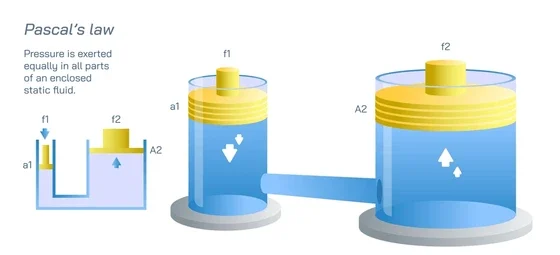
If ice numbs, compression circulates. Compression works by applying external pressure to redistribute interstitial fluid, promoting venous and lymphatic return.
Here, Pascal’s law applies: pressure applied to a fluid is transmitted equally in all directions. When a compressive sleeve, bandage, or pneumatic device is applied distal-to-proximal, it harnesses this principle to “push” fluid upward toward central circulation.
“Compression devices and stockings do not fight biology. They harnesses physics to support circulation.”
Evidence supports compression as one of the most effective methods for edema management. In a landmark study of foot and ankle trauma, intermittent pneumatic compression reduced swelling 47% within 24 hours, compared to 33% with continuous cryotherapy and just 17% with ice packs (Stöckle et al., 1997). By day four, pneumatic compression achieved a 74% reduction, outperforming cryotherapy and cool packs.
This highlights a key idea: swelling isn’t best managed by cooling tissues, it’s managed by moving fluid.
Hydrostatic Pressure & Aquatic Therapy
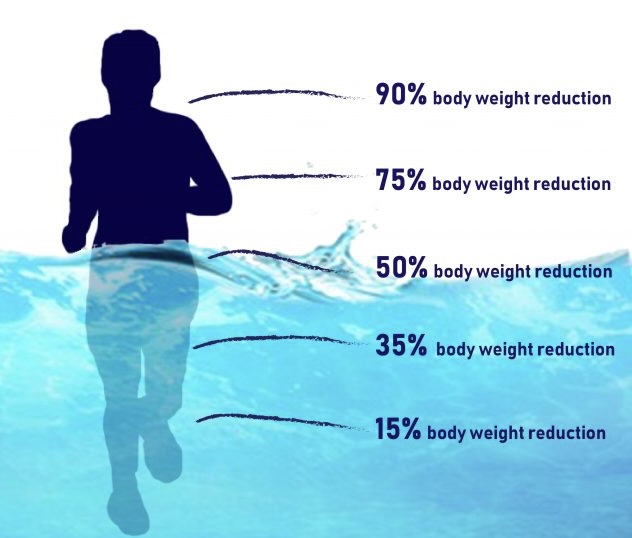
Step into a pool and physics starts working for you. Hydrostatic pressure is the force exerted by a fluid and creates a natural compression gradient on the body. The deeper you go, the greater the pressure.
At waist depth, bodyweight is reduced by ~40%. At chest depth, by ~60%. At shoulder depth, by ~85% (Torres-Ronda & Schelling, 2014). This buoyancy off-loads joints while the surrounding pressure promotes circulation.
For swelling, aquatic therapy provides a double advantage: off-loading to reduce stress on tissues and pressure to drive fluid centrally. Add movement, and you create a dynamic environment that accelerates venous and lymphatic return.
Hydrotherapy treadmills and aquatic gait training leverage these principles to provide early mobility without overloading tissues. For athletes, water becomes both a compressor and a circulation enhancer.
Movement, Muscle Pump, and Circulation
Of all interventions, movement is king.
Every muscle contraction acts like a peripheral pump, squeezing veins and lymphatic vessels to push fluid centrally. This is why even light, non-painful movement can dramatically reduce swelling compared to strict rest (Bleakley et al., 2010).
Ankle pumps, stationary cycling, or aquatic walking are not just “safe exercises”—they are biological pumps that restore circulation. The takeaway is clear: when in doubt, move what you can.
Think of swelling as a traffic jam. Ice is the stoplight as it pauses the flow but doesn’t solve congestion. Compression is the detour, redistributing cars onto side roads. Movement, however, is opening more lanes on the highway, restoring flow at its source.
Nociception, Pain, and the Role of Ice
Swelling itself can amplify pain. As inflammatory mediators build, they activate nociceptors and increase sensitivity. This is protective, but also limiting.
Ice reduces pain perception by slowing conduction along sensory nerves (Allan et al., 2022). This can be incredibly valuable in acute phases—especially when pain prevents movement. But over reliance on ice risks blunting the very inflammatory cascade needed for repair.
In modern rehab, we view ice not as the villain, but as a tool with context. Use it to manage pain in the short-term, not as a crutch that replaces circulation-based strategies.
Devices as Artificial Movement
When movement is contraindicated such as immediately post-op or with unstable injuries then technology can provide the “muscle pump effect.”
Neuromuscular electrical stimulation (NMES) devices, such as FireFly and MarcPro, deliver small contractions that mimic natural muscle pumping. These contractions stimulate circulation and promote clearance of swelling when voluntary movement isn’t yet safe.
Similarly, pneumatic compression boots and Game Ready systems combine compression with intermittent pressure and cooling. In total knee arthroplasty patients, these systems have shown improvements in swelling reduction and pain compared to standard cryotherapy (Kullenberg et al., 2006).
The principle is simple: when you can’t move, make the muscle move for you.

Protocol for Managing Swelling
So, what’s the practical roadmap?
- Prioritize safe movement: Non-painful ankle pumps, stationary cycling, or aquatic walking should be first-line strategies.
- Add compression: Elastic wraps, JOBST stockings, or pneumatic compression devices enhance fluid clearance.
- Use ice for pain control only: Helpful for nociception but not a primary tool for swelling clearance.
- Leverage devices when needed: FireFly, MarcPro, or pneumatic systems bridge the gap when movement isn’t possible.
Evidence consistently shows that swelling reduction is fastest with movement and compression, not cooling alone (Stöckle et al., 1997; Côté et al., 1988).
“Circulation beats cooling. Movement and compression are the real medicine.”
The New Era of Injury Management
The story of swelling management has evolved. Once dominated by RICE and ice bags, we now recognize that swelling is not the enemy, it’s biology at work. The true task is managing it wisely.
5 Key Summary Points
- Swelling is biology’s repair signal, not the enemy.
- Circulation, not cooling, drives fluid clearance.
- Compression leverages physics to accelerate venous & lymphatic return.
- Aquatic therapy amplifies circulation with less load.
- Pain control ≠ swelling control and movement is the true medicine.
Swelling is like traffic congestion. You don’t fix it by freezing the cars in place. You fix it by redirecting flow, opening more lanes, and keeping movement alive. Ice can still play its role, but injury recovery belongs to movement and circulation.
FREE DOWNLOAD
Start Optimizing Your Stem Cell Recovery Today with this Recovery Guide!
Watch More Like This
Read More Like This
Related Podcasts
References
Dubois B, Esculier JF. Soft-tissue injuries simply need PEACE and LOVE. Br J Sports Med. 2020;54(2):72-73Dubois. Soft-tissue injuries si….
van den Bekerom MPJ, Struijs PAA, Blankevoort L, et al. What is the evidence for rest, ice, compression, and elevation therapy in the treatment of ankle sprains in adults? J Athl Train. 2012;47(4):435-443What Is the Evidence for Rest, ….
Allan R, Malone J, Alexander J, et al. Cold for centuries: a brief history of cryotherapies. Eur J Appl Physiol. 2022;122:1153-1162Cold for centuries a brief hist….
Côté DJ, Prentice WE Jr, Hooker DN, Shields EW. Comparison of three treatment procedures for minimizing ankle sprain swelling. Phys Ther. 1988;68(7):1072-1076Comparison of Three Treatment P….
Butler D, Moseley L. Explain Pain. Adelaide, Australia: Noigroup Publications; 2003Explain_Pain_Butler.
Torres-Ronda L, Schelling X. The properties of water and their applications for training. J Hum Kinet. 2014;44:237-248Torres-Ronda.Watertraining.JHK.
Stöckle U, Hoffmann R, Schütz M, et al. Fastest reduction of posttraumatic edema: continuous cryotherapy or intermittent impulse compression? Foot Ankle Int. 1997;18:432-438.





