Approximate Read Time: 20 minutes
“Hamstring strains heal in phases—true recovery requires aligning biology with training that restores both strength and sprint capacity.”
What You will learn
- The biology of hamstring injuries and healing timelines.
- How injury classification guides rehab timelines.
- Training strategies: eccentric, isometric, neuromuscular.
- Sprint progressions for return to play.
- Metrics that matter for safe return.
Why Hamstring Strains Matter
If you’ve ever sprinted and felt a sudden pull in the back of your leg, you’re not alone. Hamstring strains are among the most common injuries in sport, representing nearly 10% of all time-loss injuries in field-based sports like soccer, football, and track (Maniar et al., 2023; Diemer et al., 2021). For athletes, this means missed training, missed competition, and the frustration of starting over. What’s worse, recurrence rates range anywhere from 15% to 70% (Ekstrand et al., 2023; Andrews et al., 2025).
Despite decades of research and the introduction of preventative programs like the Nordic hamstring curl, injury rates have not meaningfully declined (Ekstrand et al., 2023). That tells us one thing: successful recovery isn’t just about getting stronger — it’s about respecting the biology of muscle healing, understanding how injuries are classified, and aligning training to the specific demands of sprinting.
This article unpacks the science of hamstring recovery — from how the muscle heals to why certain exercises protect better than others — and outlines how to safely progress back to sprinting and sport.
“Hamstring rehab isn’t just time off — it’s biology plus training done in the right sequence.”
The Healing Phases of a Hamstring Strain

Muscle recovery doesn’t follow a simple straight line. Instead, it progresses through three overlapping phases: inflammation, proliferation, and remodeling. Understanding these timelines helps explain why coming back too early almost guarantees a setback.
Inflammatory Phase: 0–7 Days
Right after injury, the body activates its cleanup crew. Immune cells like macrophages and neutrophils arrive at the site to clear damaged fibers and release cytokines — signaling molecules that recruit muscle stem cells (satellite cells) to begin the repair process (Andrews et al., 2025). This is the stage when swelling, pain, and stiffness are most obvious. While movement is important, too much stress in this period risks disrupting the clean-up and repair process.
Proliferative Phase: 7–21 Days
This phase is the danger zone because the athlete starts to feel better with less pain, yet the muscle tissue is still not ready. In this stage, satellite cells mature into myoblasts (muscle cells), which fuse into new muscle fibers. Fibroblasts lay down type III collagen, a weaker, less organized version of the connective tissue that gives muscles structure. This scaffolding restores some integrity but is fragile, meaning the muscle is still highly susceptible to re-injury if overloaded (Andrews et al., 2025) too soon.
Remodeling Phase: 21+ Days
As healing continues, collagen fibers shift from type III to type I collagen, which is stronger and aligned with the lines of stress placed on the muscle. At the same time, neuromuscular junctions reform, restoring the ability to contract and coordinate effectively (Andrews et al., 2025). Recovery progress at this stage is dictated by how well the muscle tolerates gradual load, especially eccentric and sprint-specific forces.
The key lesson: healing is biology-driven, not just calendar-driven. Two athletes may both have a “three-week hamstring,” but their ability to return safely depends on how well their tissue remodels under progressive stress.
Why Injury Classifications Matter
Not all hamstring strains are created equal. Some are mild and heal in a week or two. Others are severe, involving tendon damage, and may sideline you for months. That’s why classification systems exist — they help doctors, therapists, and coaches set realistic expectations for recovery and guide treatment strategies.
Traditional Grades I–III
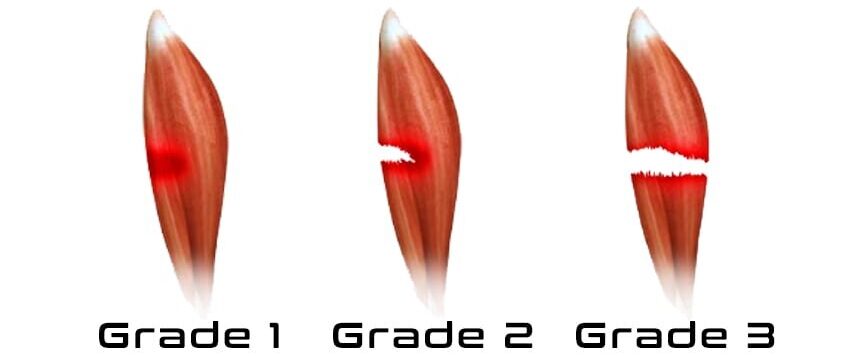
The simplest and most common system divides strains into three grades:
- Grade I: Microscopic tears with little swelling or strength loss. Often feels like tightness or mild pain. Recovery can be as quick as 1–2 weeks.
- Grade II: Partial tear of the muscle fibers. Pain is stronger, swelling is noticeable, and strength is reduced. These typically take 3–6 weeks to heal.
- Grade III: A complete tear or rupture, sometimes involving the tendon. These are severe injuries that may require surgery and several months of rehab (Ekstrand et al., 2016).
While this system is helpful, it’s broad and doesn’t always explain why some athletes recover faster or slower than others.
British Athletics Muscle Injury Classification
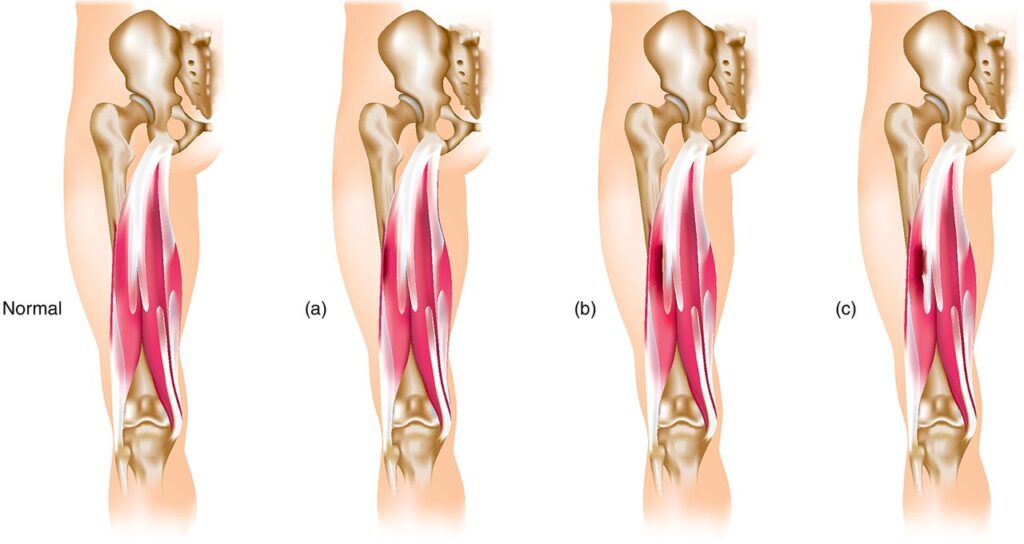
This system adds more detail by considering where in the muscle the injury occurs. It grades injuries from 0–4, and each grade has a letter attached — a, b, or c — to describe whether the tear is in the muscle belly, at the junction between muscle and tendon, or inside the tendon itself (Pollock et al., 2014).
- “a” injuries (myofascial): Closer to the surface, often heal quicker.
- “b” injuries (musculotendinous): At the junction where muscle meets tendon.
- “c” injuries (intratendinous): Involving the tendon, usually slower to heal and more likely to re-injure.
This level of detail matters. For example, two athletes might both have a “Grade II” tear. But if one is a Grade IIa(muscle only) and the other a Grade IIc (into the tendon), their rehab timelines will look very different — weeks versus months.
Munich Consensus Classification
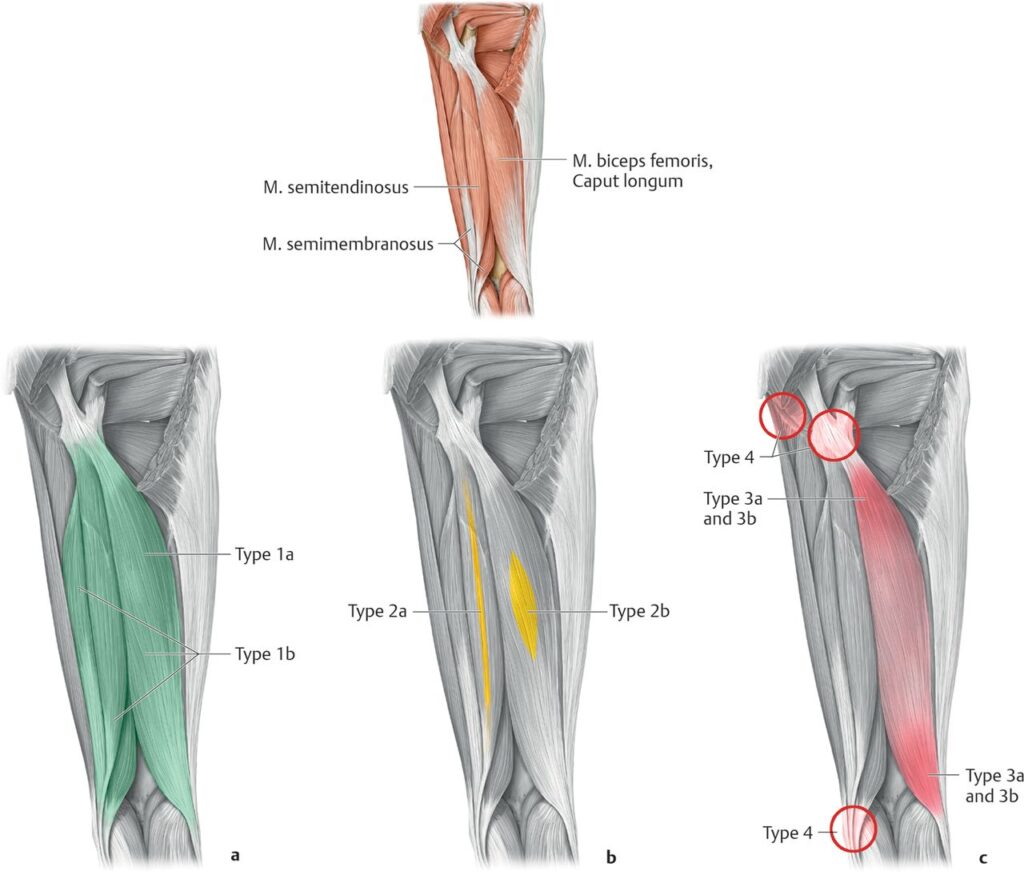
The Munich system zooms out even further. It separates injuries into two big categories: functional (issues with how the muscle works) and structural (actual tears visible on imaging) (Mueller-Wohlfahrt et al., 2013).
- Functional disorders include things like fatigue-related tightness, neuromuscular control issues, or spine-related problems that irritate the hamstrings. These don’t always show up on MRI but can limit performance and often precede true muscle tears.
- Structural injuries include partial and complete tears (Types 3 and 4).
This approach reminds us that not all hamstring pain equals a tear. Sometimes the problem is coordination, fatigue, or the spine. Addressing these functional issues can prevent them from progressing into a more serious strain.
Why These Systems Matter to You
For athletes and active adults, the takeaway is simple: the label given to your injury helps predict your recovery timeline and guides the intensity of your rehab. A tendon-involved injury (like a Grade IIc) almost always takes longer to heal than a simple muscle strain (like a Grade IIa). Functional injuries may require addressing fatigue, pelvic control, or even spine mechanics before layering on heavy hamstring work.
“A Grade II isn’t always the same — the location and type of tissue involved determine how fast you’ll recover.”
Hamstrings in Sprinting
Most hamstring strains don’t happen while jogging or warming up. They occur during sprinting at top speed, especially in the late swing phase — that split second before your foot strikes the ground.
During this phase, the hamstrings act like high-tension brakes. They contract eccentrically (lengthening under load) to decelerate the swinging leg and prepare for ground contact. The demands are enormous: the hamstrings must absorb force while already stretched close to their maximum length (Schache et al., 2012).
Why the Biceps Femoris Long Head Is Vulnerable
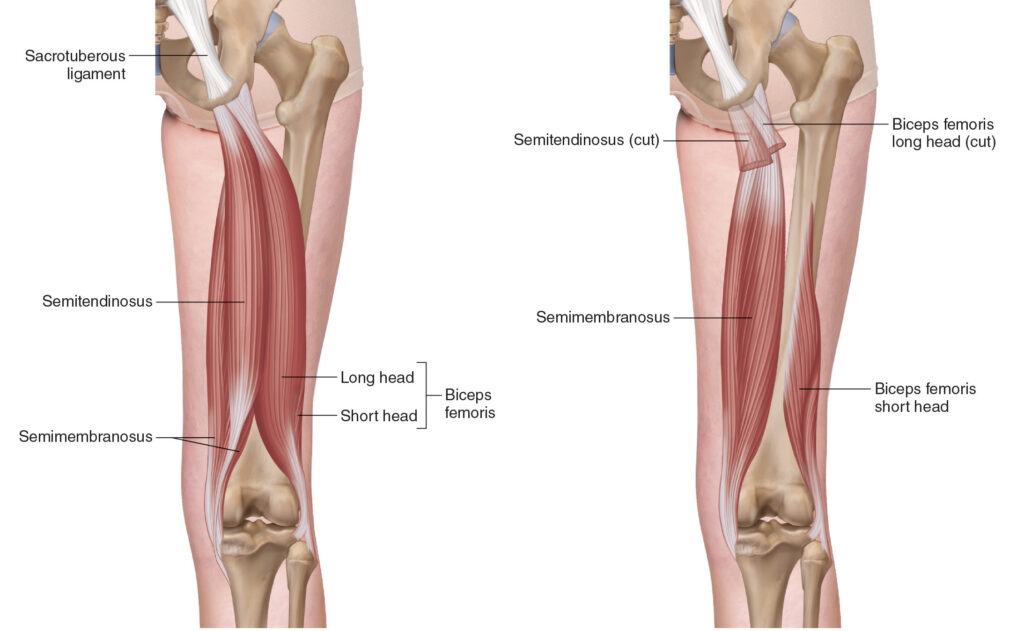
Of the three main hamstring muscles, the biceps femoris long head (BFlh) is most often injured. Research shows it experiences the largest musculotendon strain during late swing, and peak strain occurs earlier than in the semitendinosus or semimembranosus (Schache et al., 2012).
A prospective study found that athletes with shorter BFlh fascicles (<10.56 cm) were over four times more likely to suffer a hamstring strain than those with longer fascicles (Timmins et al., 2016). Likewise, athletes with eccentric hamstring weakness were also at higher risk (Opar et al., 2015). In plain terms: shorter and weaker hamstring equal greater injury odds.
Fatigue, Neural Timing, and Force
It isn’t just muscle architecture. Neural control plays a huge role. If the hamstrings activate too late or generate too little force, they can’t resist the rapid forward momentum of the leg (Andrews et al., 2025). This explains why even strong athletes pull up when sprinting late in games — fatigue affects the nervous system as much as the muscle.
When you combine long stride length, high running speed, and fatigued or weak hamstrings, the recipe for strain is set. This is why most injuries occur at high speed rather than during gym exercises — the forces, velocities, and coordination demands are simply higher.
Rehab & Training: Old and New Perspectives
The Classic Approach: Eccentric Strengthening
For years, eccentric exercises have been the cornerstone of hamstring rehab. The most famous example is the Nordic Hamstring Curl. By resisting your bodyweight as you slowly lower forward, you lengthen the hamstrings under high load.
Why does this matter? Eccentric training is proven to:
- Increase fascicle length: Shorter fascicles are linked to higher injury risk. Nordics promote sarcomerogenesis (adding sarcomeres in series), effectively lengthening the muscle to handle stretch during sprinting (Timmins et al., 2016; Opar et al., 2015).
- Improve tensile strength: Eccentric contractions produce more force than concentric ones, preparing hamstrings to absorb the high loads of late-swing sprinting (Andrews et al., 2025).
- Promote neural adaptations: Eccentric exercises enhance motor unit recruitment, critical for controlling deceleration at high speeds (Opar et al., 2015).
Meta-analyses show that programs including Nordics can reduce hamstring injury rates by 50–70% (van Dyk, Behan, & Whiteley, 2019). Still, eccentric training is not the whole story.

The Modern Layer: Isometrics and Neuromuscular Adaptations
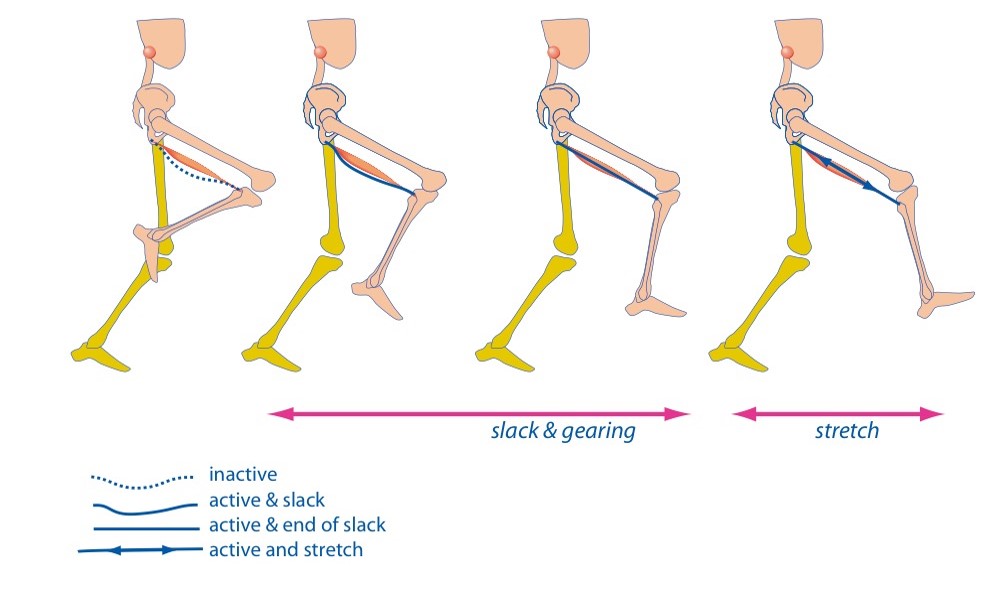
Sprint mechanics reveal that the hamstrings act nearly isometric during the terminal swing phase, while the tendon and connective tissues absorb and recoil energy (Schache et al., 2012). That means replicating this behavior in training may better prepare athletes for sprint demands.
- Reduce muscle slack: Slack refers to the delay before force is transmitted through connective tissues. Isometric holds stiffen the system, improving readiness for rapid force (van Hooren & Bosch, 2017).
- Enhance elastic behavior: High-intensity isometric holds mimic how hamstrings function in sprinting — stiff, reactive, and forceful.
- Improve stability: Exercises like isometric glute-ham holds or single-leg bridges with perturbations challenge dynamic stability at the hip and knee.
Neuromuscular control is equally critical. Training coordination between hamstrings, glutes, and adductors restores the body’s ability to stabilize the pelvis and control stride mechanics. Perturbation drills and rotational single-leg exercises can retrain this coordination, reducing re-injury risk (Andrews et al., 2025).
Blending Classic and Modern
The most effective programs combine the strengths of both approaches:
- Eccentrics lengthen the hamstrings and build raw strength.
- Isometrics prepare the muscle-tendon unit for sprint-specific demands.
- Neuromuscular drills integrate control and coordination.

For example, you might pair Nordics with isometric glute-ham raises at near-straight knee angles, then progress to sprint drills with perturbations. This synergy ensures the hamstring isn’t just strong — it’s functionally prepared for sprinting chaos.
“Eccentrics build the brakes, isometrics reduce the slack, and neuromuscular training teaches the system how to use both.”
Running Progressions: From Control to Chaos
Rehab doesn’t stop in the gym. To return safely to sport, you must reintroduce running and sprinting step by step, matching the demands of the healing muscle to the forces of sport. Sprinting exposes hamstrings to their highest loads, so progression here is critical.
Early Phase: Controlled Running & Long Contacts
- Marching drills and sled pushing help re-establish running mechanics by slowing the movement down and increasing ground contact times.
- Short accelerations (5 – 10 m) at moderate intensity build confidence and minimize the eccentric demands of sprinting or deceleration.
- These early sessions emphasize concentric actions (pushing off the ground) with less eccentric stress, protecting the healing hamstring (Taberner, Allen, & Cohen, 2019).
Mid Phase: Adding Stress
- Introduce resisted sprints (light sleds, resistance bands) to slow athletes down while still producing high force.
- Layer in lateral shuffles and planned changes of direction to introduce multidirectional demands.
- Volume and velocity gradually increase, but exposures to >80% max sprint remain limited.
Late Phase: High-Speed and Chaos
- Progress to straight-line sprints at >90% speed, since true sprinting is the ultimate hamstring test (Schache et al., 2012).
- Add unanticipated drills — reactive sprints, unpredictable changes of direction, and small-sided games — to mirror the chaos of sport (Taberner et al., 2019).
- By this point, the hamstring must tolerate maximal stretch, maximal speed, and rapid coordination demands.
The Control-Chaos Continuum
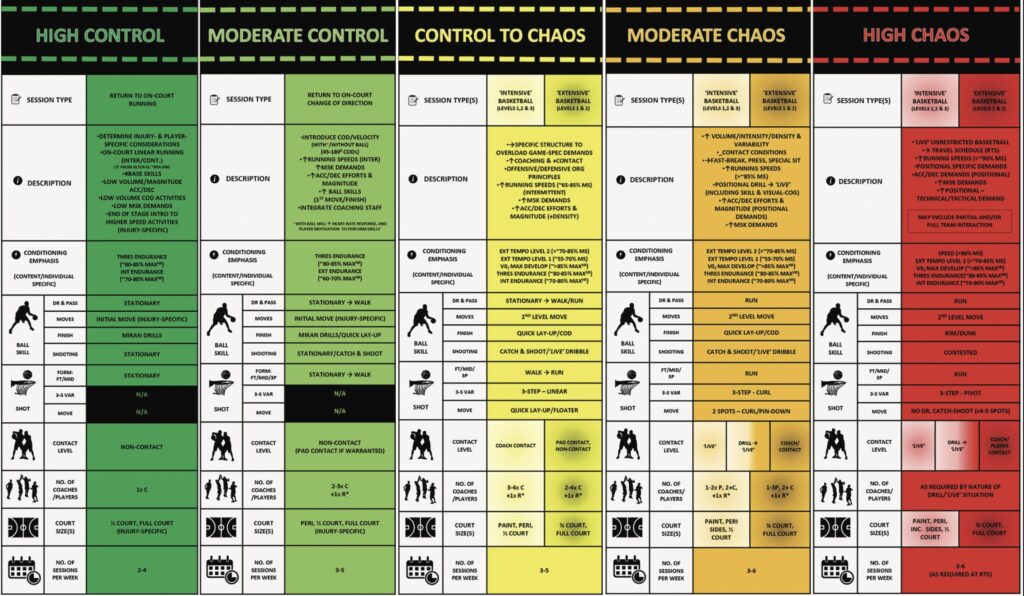
A practical framework for this progression is the Control-to-Chaos Continuum (Taberner et al., 2019). Early drills emphasize control: predictable, low-variability movements like linear running. As rehab advances, layers of chaos — spontaneity, reactive drills, and game-like situations — are gradually introduced.
The value of this continuum is that it mirrors the reality of sport. Athletes rarely get hurt in controlled environments. Injuries strike during chaotic, unplanned moments: reacting to an opponent, chasing a ball, or making a last-second cut. Preparing the hamstring for this chaos is essential to reduce recurrence.
Metrics That Matter
Alongside progression, measuring recovery ensures readiness:
- Strength symmetry: Eccentric and isometric hamstring force within 10% of the opposite side (Opar et al., 2015).
- Hamstring-to-Quadriceps ratio: ≥65% to reduce reinjury risk (Timmins et al., 2016).
- High-speed running exposure: Accumulated sprint volume >5.5 m/s before returning to games (Andrews et al., 2025).
- Pain-free ROM: Full, comfortable motion during straight-leg raise or knee extension.
“The hamstring must prove itself at full speed and under chaos — not just in the weight room.”
Conclusion: Healing Meets Performance
Hamstring rehab is more than resting until the pain fades. It’s a process that blends biology, training, and sprint-specific preparation. Muscles heal through inflammation, proliferation, and remodeling — and this timeline must be respected. Classification systems add precision, showing that not all “Grade II” injuries are the same.
In sprinting, the hamstrings are prone to injury during late swing because they’re asked to absorb enormous forces at long lengths. That’s why fascicle length and eccentric strength are so critical, and why eccentric training like Nordics has such strong protective evidence. But sprinting also reveals the importance of isometric control, elastic recoil, and neuromuscular coordination, which modern rehab strategies now embrace.
Finally, no hamstring rehab is complete without sprinting itself. Using frameworks like the Control-to-Chaos Continuum, athletes can be safely progressed from controlled drills to unpredictable, game-like movements that mimic real demands. By respecting biology, applying smart training, and monitoring key metrics, the risk of re-injury falls — and athletes can return to sport with confidence.
“Strong hamstrings are not enough — they must be long, fast, and ready for chaos.”
The Fab Five: Key Takeaways
- Healing Phases Matter: Hamstrings progress through inflammation, proliferation, and remodeling — rushing these stages increases reinjury risk.
- Classification Adds Precision: Systems like British Athletics and Munich Consensus reveal why tendon-involved strains heal slower.
- Fascicle Length + Eccentric Strength: Short fascicles and weak eccentrics raise injury risk.
- Blend Old and New: Nordics build fascicle length; isometrics reduce slack and mimic sprint demands.
- Control to Chaos: Return-to-play requires progressing from controlled runs to chaotic, game-like sprint exposures.
Free Download
Watch More Like This
Read More Like This
Related Podcasts
References
Andrews, M. H., Shield, A. J., Lichtwark, G. A., & Pincheira, P. A. (2025). Hamstring injury mechanisms and eccentric training-induced muscle adaptations: Current insights and future directions. Sports Medicine.
Bourne, M. N., Duhig, S. J., Timmins, R. G., Williams, M. D., Opar, D. A., Al Najjar, A., & Shield, A. J. (2017). Impact of the Nordic hamstring and hip extension exercises on hamstring architecture and morphology: Implications for injury prevention. British Journal of Sports Medicine, 51(5), 469–477.
Ekstrand, J., Lee, J. C., & Healy, J. C. (2016). MRI findings and return to play in football: A prospective analysis of 255 hamstring injuries in the UEFA Elite Club Injury Study. British Journal of Sports Medicine, 50(12), 738–743.
Maniar, N., Carmichael, D. S., Hickey, J. T., Timmins, R. G., San Jose, A. J., Dickson, J., & Shield, A. J. (2023). Incidence and prevalence of hamstring injuries in field-based team sports: A systematic review and meta-analysis of 5952 injuries. British Journal of Sports Medicine, 57(2), 109–116.
Opar, D. A., Williams, M. D., Timmins, R. G., Hickey, J., Duhig, S. J., & Shield, A. J. (2015). Eccentric hamstring strength and hamstring injury risk in Australian footballers. Medicine & Science in Sports & Exercise, 47(4), 857–865.
Schache, A. G., Dorn, T. W., Blanch, P. D., Brown, N. A., & Pandy, M. G. (2012). Mechanics of the human hamstring muscles during sprinting. Medicine & Science in Sports & Exercise, 44(4), 647–658.
Taberner, M., Allen, T., & Cohen, D. D. (2019). Progressing rehabilitation after injury: Consider the ‘control-chaos continuum’. British Journal of Sports Medicine, 53(18), 1132–1136.
Timmins, R. G., Bourne, M. N., Shield, A. J., Williams, M. D., Lorenzen, C., & Opar, D. A. (2016). Short biceps femoris fascicles and eccentric knee flexor weakness increase the risk of hamstring injury in elite football (soccer): A prospective cohort study. British Journal of Sports Medicine, 50(24), 1524–1535.





