Approximate Read Time: 14 minutes
“Not all PRP is created equal—age, preparation, and formulation matter more than we ever thought.”
What You will learn
- PRP has evolved from a simple blood spin to a biologic tool with nuanced subtypes.
- Variants like leukocyte-rich, leukocyte-poor, PRP-Plus, and A2M have unique clinical effects.
- Aging influences PRP efficacy, especially in joint and tendon healing.
- PRP is not interchangeable—lab processing quality and cellular content matter.
- PRP should be considered alongside MSCs, BMAC, peptides, and exosomes for a tailored biologic strategy.
Introduction: PRP—From Buzzword to Biotech
At one point, PRP was seen as the miracle cure—a simple blood draw, a quick spin, and an injection that promised to regenerate joints and heal tendons. Its rise to fame was fueled by high-profile athletes and the idea that we could heal using our own biology. But in the years since its introduction, PRP has become at times misunderstood yet evolved to support musculoskeletal medicine.
This article unpacks how PRP has evolved, why its formulation matters, how age influences its effects, and how it fits within the broader spectrum of biologics like A2M, stem cells, peptides, and exosomes.
PRP 101: What Is It, and Why Did It Gain Traction?
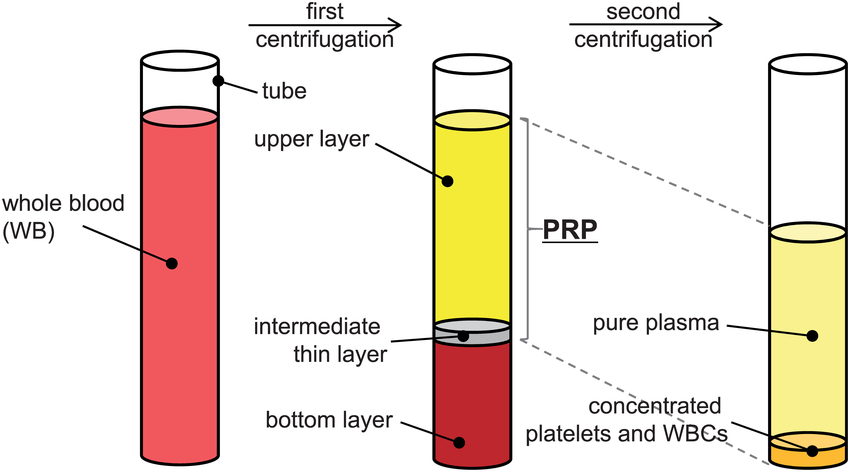
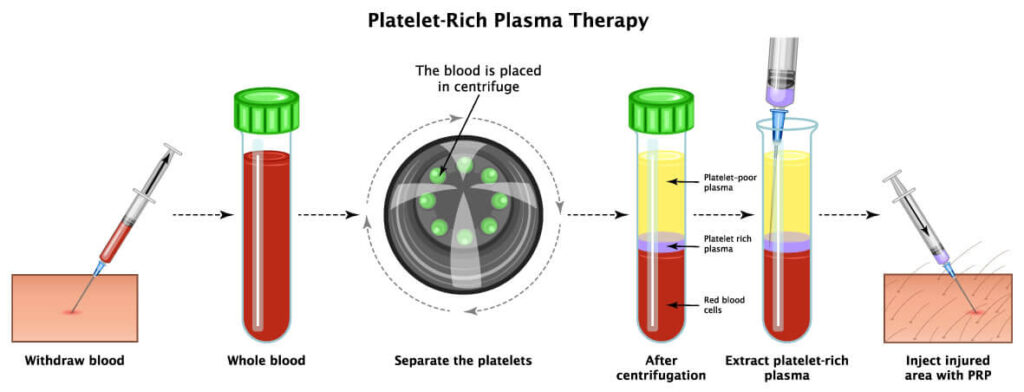
PRP, or Platelet-Rich Plasma, is derived from your own blood. After a centrifuge process separates red blood cells and plasma, what’s left is a concentrated mix of platelets. These platelets release growth factors that are involved in inflammation modulation, cell migration, and tissue repair.
“PRP isn’t one product—it’s a category.”
Originally used in oral surgery and wound care, PRP gained traction in sports medicine around the 2000s. Its appeal was simplicity: autologous, outpatient, and low risk. But the clinical community quickly realized one thing: not all PRP is created equal.
Not All PRP Is Created Equal
Each variation can have dramatically different effects based on how it’s prepared—which centrifuge is used, what speed and time, and whether it’s single or double spun. Let’s review some of the common variations and their clinical indications:
- Leukocyte-Rich PRP (LR-PRP): Contains white blood cells; pro-inflammatory; often used in tendinopathies.
- Leukocyte-Poor PRP (LP-PRP): Lacks white blood cells; anti-inflammatory; used in joints and intra-articular injections.
- PRP-Plus: Enriched with higher platelet counts and specific growth factor ratios.
- A2M (Alpha-2-Macroglobulin): A plasma protein added to PRP to neutralize cartilage-degrading enzymes like MMPs.
Age and PRP: Why Young Blood Might Be Better
The more I learn about orthobiologics, the more I am learning of the subtle nuances that lie within. One of those nuances is how age may, or may not, impact the efficacy of PRP. Recent studies have shown that age is more than a just number when it comes to PRP efficacy:
- A 2023 study by Chowdhary et al. found that PRP from young donors significantly enhanced chondrogenesis in vitro and improved cartilage integrity in vivo. PRP from older donors, however, failed to stimulate repair and may have even provoked inflammation
- Berger et al. (2019) showed that tenocyte response to platelet lysate was concentration-dependent in aged donors, whereas young donor cells responded similarly across concentrations. This suggests that platelet dosing and age interact in complex ways.
When reviewing these two of many articles, I have drawn the conclusion that the answer to “does age matter?” is not so cut and dry. Yes, it does matter, and no it does not if you have a process that can increase the concentrations for older individuals.
Like many things in the world of longevity and regenerative medicine, the details matter.
PRP for Acute vs. Chronic Injuries: Has the Pendulum Swung?
In its early days, platelet-rich plasma (PRP) gained traction as a promising treatment for chronic tendinopathies and mild osteoarthritis—particularly among athletic populations looking for non-surgical solutions. But today, the evidence is more nuanced. While the initial excitement has tapered for use in chronic joint degeneration, there is growing support for PRP as a tool for early intervention, especially when integrated into a well-designed rehab plan.
Clinical outcomes also appear to be influenced by patient demographics. Younger, healthier individuals with less systemic inflammation tend to respond more favorably to PRP treatment, suggesting that biologic therapies may not be universally effective without personalization.
For older adults—especially those over 60 with advanced osteoarthritis—the use of PRP remains a topic of debate. Its benefits in this population appear limited without precise ultrasound guidance or a carefully tailored PRP formulation.
“PRP might not be a miracle—but with the right patient and formulation, it’s powerful medicine.”
PRP vs. BMAC vs. Stem Cells vs. Peptides vs. Exosomes
The biologics landscape is rapidly expanding, but not all options serve the same purpose—or patient. This table offers a side-by-side comparison of PRP, A2M, BMAC, MSCs, peptides, and exosomes, outlining where each fits in the spectrum of regenerative care. From source and delivery to mechanism and regulatory status, it’s a snapshot of what today’s clinicians and patients need to navigate personalized recovery.
| Biologic | Source | Target Use | Mechanism | FDA Status |
|---|---|---|---|---|
| PRP | Autologous blood | Joints, tendons | Growth factors, inflammation | Widely used |
| A2M | Plasma protein | Cartilage/OA | Protease inhibition | Adjunctive |
| BMAC | Bone marrow | Soft tissue + cartilage | Cell therapy + signaling | Investigational |
| MSCs (UC) | Umbilical cord | Systemic + joint | Immune modulation | Not FDA-approved |
| Peptides | Synthetic, biologic | Recovery, regen | Cellular signaling | Regulated |
| Exosomes | Cell secretions | Whole body + local | Messenger vesicles | Experimental |
Final Thoughts: Precision Over Hype
PRP is not a one-size-fits-all injection. Age, condition type, formulation, and how it integrates with rehab all determine its success. The future of PRP isn’t about spinning blood faster—it’s about personalizing biology.
“Biologics only work when rehab gives them a reason to.”



