Approximate Read Time: 8 minutes
“A tear on MRI doesn’t always mean the joint is unstable. Structure is part of the story. So is function.”
What You will learn
- Surgery is often offered quickly—but it’s not always the best or only path.
- Asking the right questions leads to confident, informed decisions.
- Conservative care doesn’t mean passive—it should be structured and progressive.
- Imaging and diagnosis are only part of the full story.
- The right decision is personal—it reflects your goals, values, and real-world demands.
When the Scan Says “Torn” But You’re Not So Sure
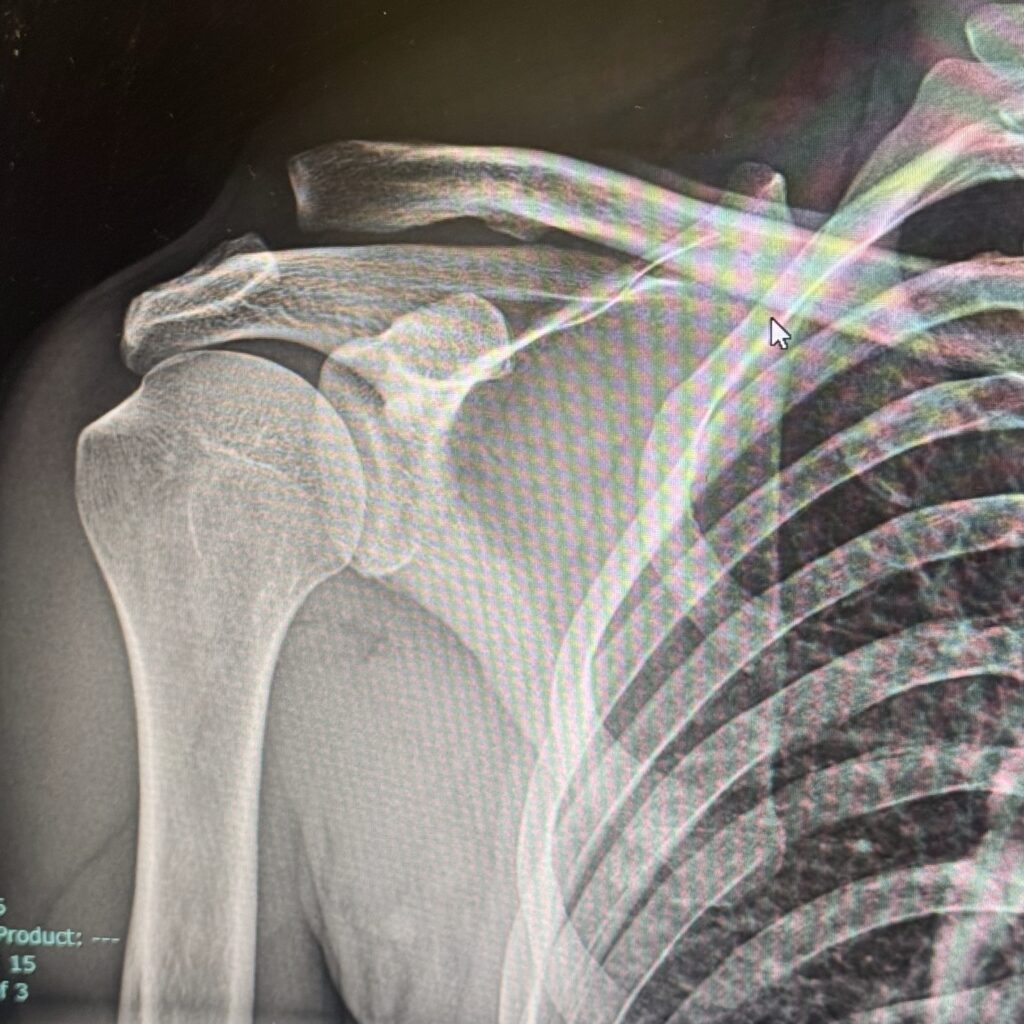
A few months ago, I stood on the other side of the treatment table—not as a performance therapist, but as a patient. I had just flipped over the handlebars of my bike and landed hard on my shoulder. An MRI confirmed a Grade III AC joint separation, and suddenly I found myself wrestling with the same decision many of my clients face: Should I get surgery or not?
The pressure to make a decision came fast—orthopedic consults, Google Scholar searches, and consulting trusted professionals. And while my clinical brain knew what to ask, my emotional brain felt overwhelmed. This is the space so many athletes and active adults find themselves in: somewhere between a diagnosis and a decision.
In this article, I want to help you bridge that space. Whether you’re dealing with a shoulder injury, a knee tear, or a spinal disc issue, these five questions can guide you through the fog of urgency and into clarity.
1. What Does the Injury Actually Need—Stability, Time, or Intervention?
Let’s start with the reality: not every tear requires a scalpel. In fact, many injuries that look severe on imaging can be managed with structured, intelligent rehab.
In my case, a Grade III AC joint separation meant complete disruption of the acromioclavicular and coracoclavicular ligaments. The bump on my shoulder was visible. But I had no numbness, no loss of strength, and no instability with basic movements. After reviewing the imaging and clinical findings with an orthopedic surgeon, we both agreed that conservative care made sense. Surgery was still on the table—but it wasn’t the only card I could play.
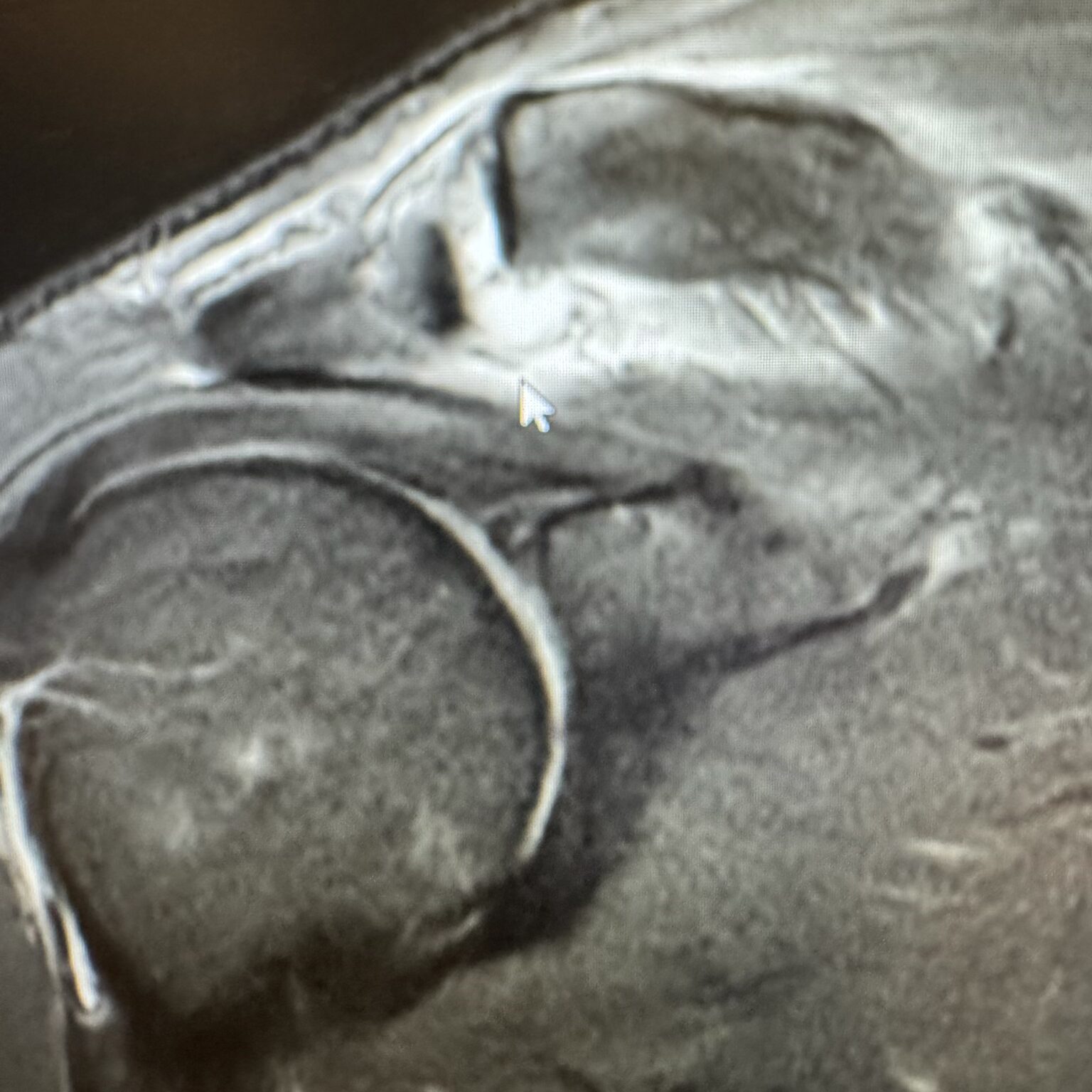
“A tear on MRI doesn’t always mean the joint is unstable. Structure is part of the story. So is function.”
Ask yourself: Is this injury something that needs surgical stabilization now—or can I give it time under skilled guidance to see how it behaves?
2. Have You Truly Explored High-Quality Conservative Care?
There’s a huge difference between rest and rehab. If your version of conservative care so far has been rest, NSAIDs, and an ice pack, you haven’t truly tested your recovery capacity.
Real conservative care involves:
- Blood Flow Restriction (BFR) training to preserve muscle
- E-stim to manage tone and initiate neuromuscular control
- Sensorimotor feedback to retrain postural systems
- Load progression through closed-chain, supported, and eventually dynamic exercises
That’s what I leaned on during my own recovery. We used BFR to limit atrophy, manual isometrics to reintroduce safe activation, and visual feedback drills to retrain scapulohumeral rhythm. None of it was passive. It was training—with constraints.
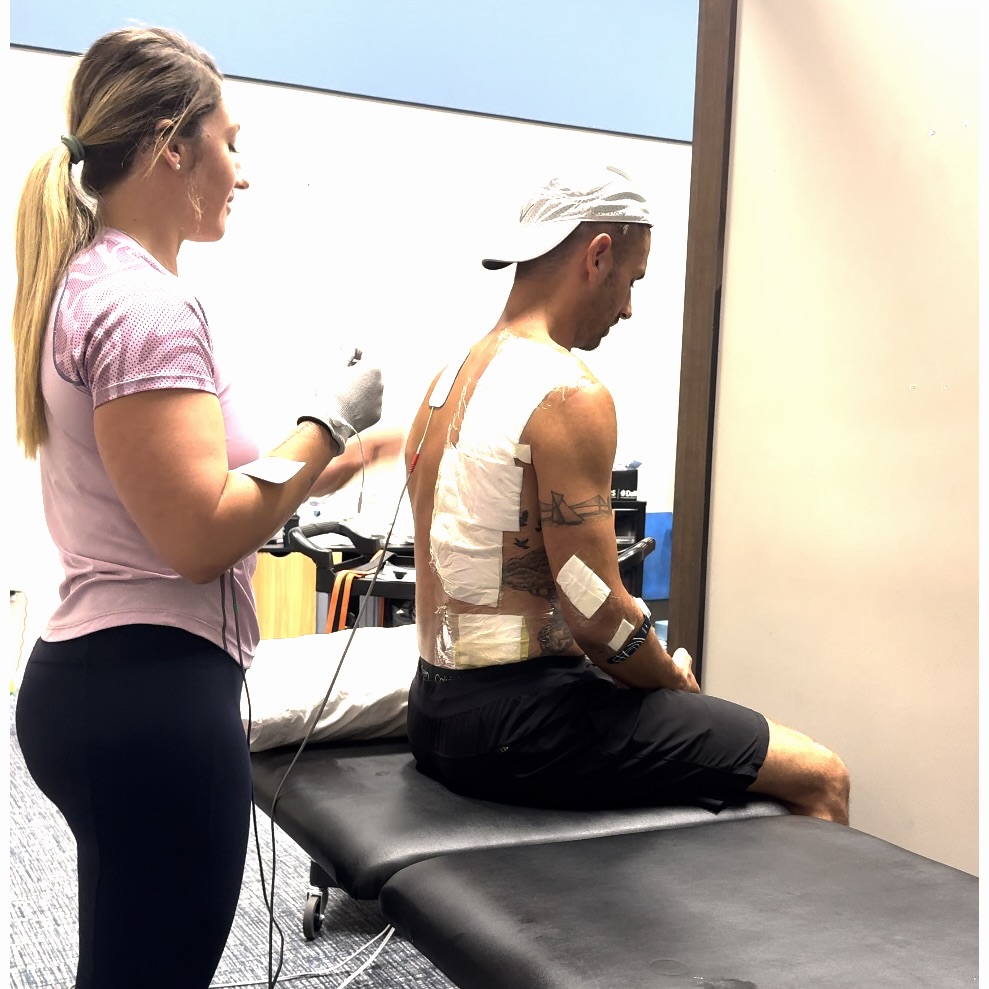
Before deciding on surgery, ask: Have I worked with a professional who knows how to build a progressive rehab plan specific to this injury and my goals?
“Rest is a temporary pause. Rehab is a forward plan. Know the difference.”
3. What Does Your Life Actually Require From This Joint?
This might be the most important question—and the one least often asked.
If you’re a competitive athlete whose sport demands high-level joint integrity (think overhead athlete, contact sport, or elite-level function), the threshold for surgical consideration may be lower. But if you’re an active adult who wants to get back to lifting, running, or playing recreational sports pain-free, function should guide your decision—not fear.
In my case, I wasn’t preparing for a combine or the Olympic trials. I needed to be able to push, pull, carry, and move with integrity—for life, family, and the long game. My shoulder didn’t need to be “perfect.” It needed to be reliable.
Ask yourself: What do I actually need this joint to do, and can that function be restored through training, not surgery?
“Surgery isn’t about fixing a structure—it’s about restoring a function you actually use.”
4. What Are the Risks of Doing It Now vs. Waiting?
Not all injuries can—or should—be rehabbed indefinitely. Some require timely intervention to prevent worsening (e.g., rotator cuff tears with retraction, labral tears with locking). But that urgency should come from clinical reasoning, not pressure.
There’s value in understanding the window of opportunity for surgical repair if needed. But there’s also value in giving the body a fair trial of movement-based healing first. Most orthopedics will support 4–6 weeks of structured rehab before considering surgery—unless there’s clear instability, locking, or nerve involvement.
Ask your provider: What would I lose by waiting 4–6 weeks while trying high-quality rehab? If the answer is “nothing,” then you’ve just bought yourself space.
“Sometimes there’s urgency. Sometimes there’s just pressure. Know which one you’re feeling.”
5. Have You Gotten a Second (or Third) Opinion From Someone You Trust?
Too often, patients accept surgery as the only option because they haven’t been offered another one. Or worse—they haven’t talked to a provider who doesn’t directly benefit from that choice.
Your decision deserves perspective. I’ve referred patients to surgery. And I’ve also talked them out of it. But both times, the decision came after education, exploration, and time.
The best medical decisions often come when multiple opinions converge around the same truth. If your surgeon, physical therapist, and trusted professional all agree surgery is the best next step—that’s meaningful. If not, keep asking.
“The best decision is the one you make when your questions have answers—not emotions.”
Final Thoughts: Reclaiming Control Over the Fork in the Road
Surgery is not failure. And rehab is not always enough. The goal of this article isn’t to steer you toward one option—but to help you own the process of deciding.
In my case, I chose conservative care. I committed to 6 weeks of structured, high-level rehab.
Maybe your path looks different. But if you ask the right questions—it will be yours.

Recommended Podcasts
- Finding Small Wins: The Science of Stretch ft. Dr. Leada Malek
- Finding Small Wins: Evolving Sports Rehab ft. Dr. Trevor Rappa