Approximate Read Time: 7 minutes
“Being the patient forced me, the physical therapist, to feel the gray space of rehab during an AC joint injury. I was reminded of the very same messages I tell my athletes during their own rehab cases.”
What You will learn
- Case study: Grade III AC joint separation managed by myself.
- Evidence-based recovery strategy using BFR and e-stim.
- Considerations for post-op vs non-op decision-making in shoulder injuries.
My Personal Story
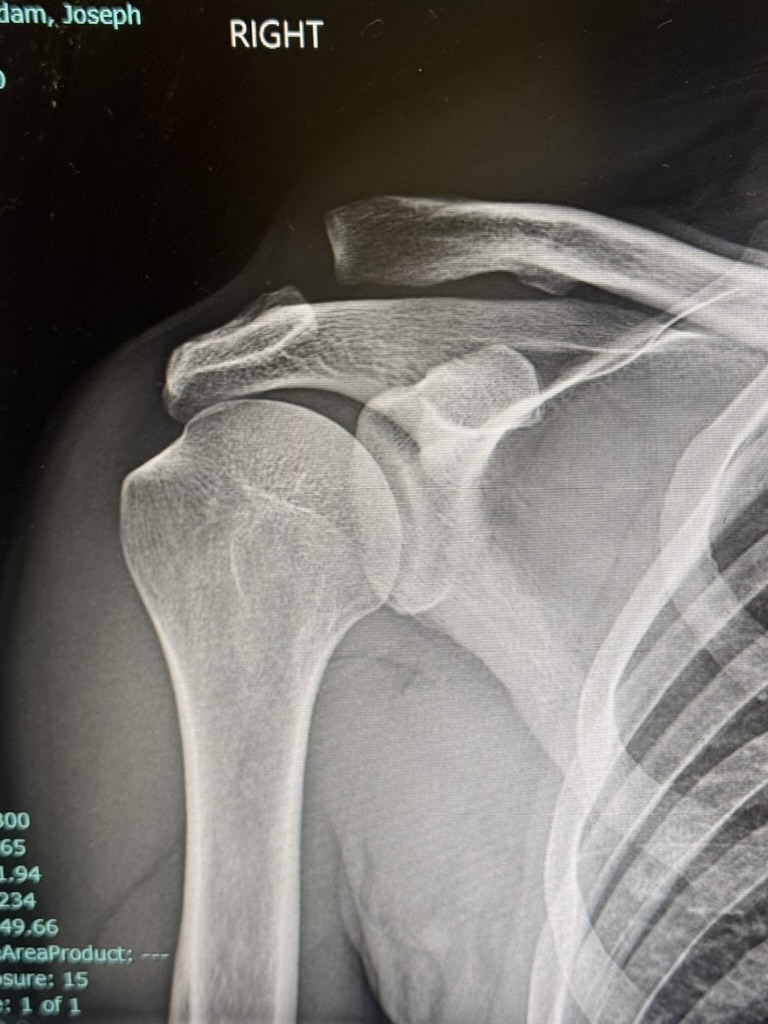
On a sunny weekend ride in Scottsdale, I flipped over the handlebars and landed squarely on my shoulder. Diagnosis: Grade III AC joint separation. For someone who has spent 15+ years helping professional athletes recover from injury, this was a moment of irony, humility, and reflection.
This article is a case study not just in shoulder rehab, but in how the body heals, how we adapt, and how even the most experienced physical therapist, coach, or athletic trainer can benefit from a lived experience.

Anatomy of AC Joint
The acromioclavicular (AC) joint connects the clavicle (collarbone) to the acromion, the highest point on the scapula. It plays a critical role in shoulder mobility and stability, particularly in overhead and cross-body movements.
AC joint separations are categorized into different types:
- Grade I: Sprain of the AC ligament without separation.
- Grade II: Partial tear of the AC ligament with slight separation.
- Grade III: Complete tear of the AC and coracoclavicular (CC) ligaments with visible deformity.
- Grade IV-VI: Increasing severity with clavicle displacement and muscle/tissue disruption, often requiring surgical management.
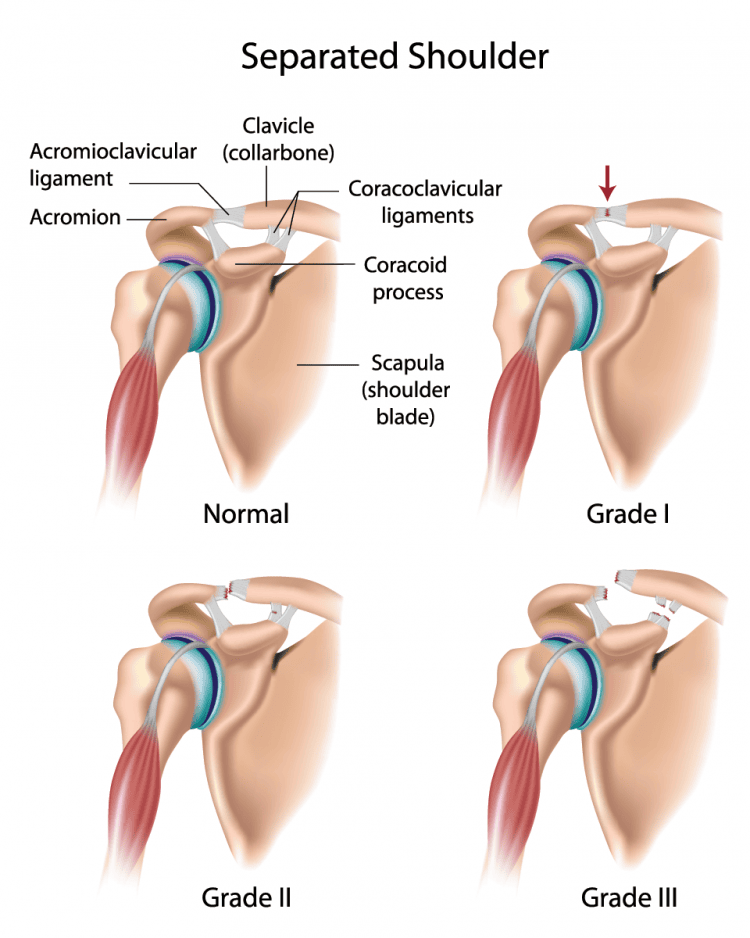
A Grade III separation disrupts both primary stabilizers, which can significantly impact the scapulothoracic rhythm. The scapula may become less stable during elevation and rotation, leading to altered muscle activation in the deltoid, trapezius, and rotator cuff.
My first 7 days after the injury were hell to say the least. I had signficant pain directly over the AC joint area and myofascial pain in the upper trapezius, middle rhomboids, and biceps tendon. This myofascial pain was because these muscles were protecting the injured area by spasming to limit mobility.
Think of muscle spasms after an injury as your own body’s response to creating a “brace” to immobilize the injured area. I honestly forgot how much of a role this plays into early rehab and how vitally important a good manual therapist can be to help reduce this tension.
AC Joint Conservative vs. Surgical Management
“Sometimes the hardest choice is not to fix, but to trust the body to rebuild.”
Following the diagnosis of an AC joint separation, I met with a both a non-operative orthopedic physician and orthopedic surgeon at Arizona Sports Medicine Center to discuss treatment options. Given the absence of horizontal instability, moderate pain at rest, and no significant overhead demands in my daily life during recovery, we agreed on a conservative approach that was a decision supported by recent research.
Part of my questioning with the doctors was discussing my goals of wanting to be able to lift heavy things for decades to come and not compromise overhead function as I age. We discussed these options and below were some of the conclusions we came to:
- No significant difference in long-term function: Multiple meta-analyses and systematic reviews report that patient-reported outcomes (e.g., Constant, DASH, ASES scores) are similar between surgical and conservative care, even at 1 year or longer follow-up
- Return to activity: Nonoperative care often allows for a faster return to work and sports, while surgery may delay this due to recovery time
- Pain and satisfaction: Pain levels and patient satisfaction are generally comparable between groups
- Aesthetics: aside from having a mild step-off deformity from the separation, we could not agree on any strong indicator that suggested to elect for surgery.


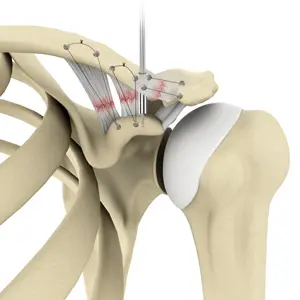
However, surgical management may have been appropriate if my job required more overhead activities or intensive manual labor. Modern surgical techniques involve anatomic reconstruction of the coracoclavicular ligaments with graft augmentation, but these often require 4 – 6 months of restricted activity. The surgeon shared his personal recommendation of let’s give it 6 weeks of conservative care, and if we are unhappy with functional outcomes then we can revisit surgery.
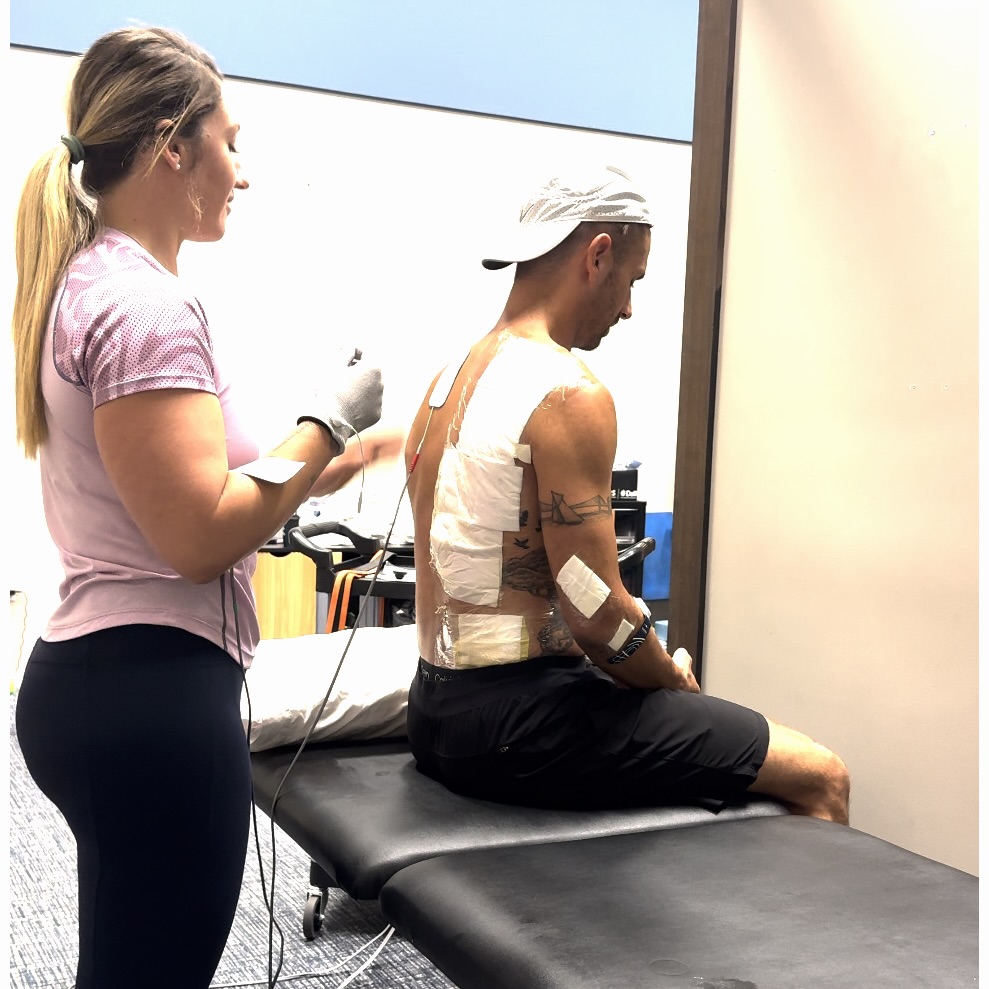
For my case, conservative care allowed immediate initiation of therapeutic strategies like BFR and e-stim while avoiding the systemic stress of surgery.
Stages of AC Joint Healing
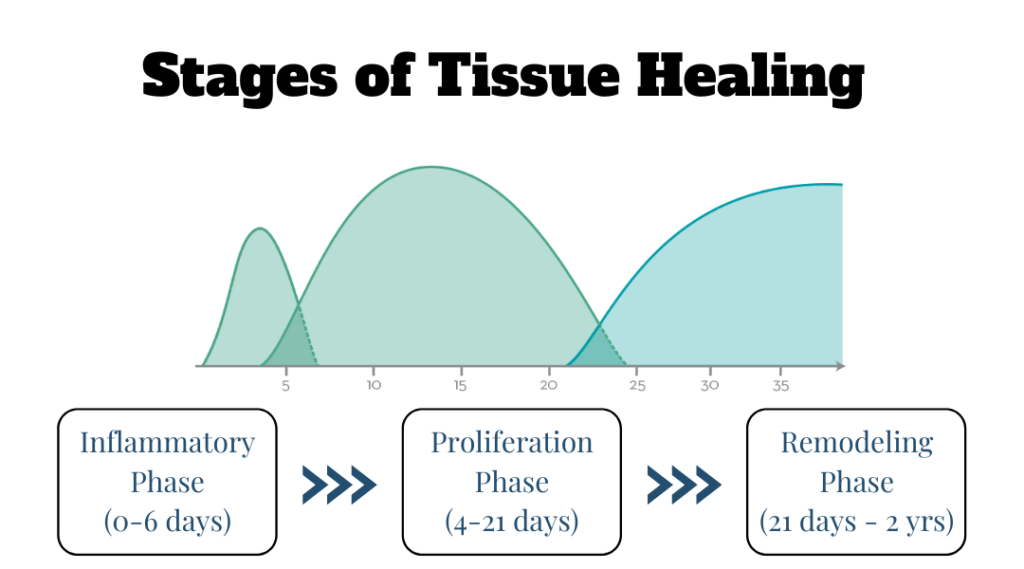
Understanding tissue healing is essential in guiding the rehab timeline. Let’s take a quick review of the key stages of healing:
- Inflammation (0-7 days): Swelling and pain dominate. Protection is key.
- Proliferation (1-3 weeks): Fibroblast activity, neovascularization, and early collagen synthesis.
- Remodeling (3-12+ weeks): Collagen matures, and tissue gains tensile strength.
The AC joint and surrounding ligamentous structures rely heavily on mechanical loading during remodeling to promote alignment and strength of newly synthesized collagen fibers. This underpins the rationale for progressive loading with BFR, isometrics, and functional movement.
AC Joint Week-by-Week Rehab Strategy
“The body needs calm before it can regain control.”
As a sports physical therapist and many resources available to me, I feel pretty confident in my ability to get back good function. My goal by 6 weeks is to have normal functional with relatively good strength. I still expect I will need probably another 4-6 weeks after this initial 4-6 weeks to get myself back to a place of where I feel the shoulder will be able to withstand high intensity activities. All in I’ve set my timeline to be about 12 weeks.
Week 1: Protect and Calm
- Sling for joint protection.
- Firefly e-stim on upper and lower arm to improve circulation.
- Pulsed e-stim (Compex) on peri-scapular and pectoral muscles to reduce spasm.

Week 2: Begin Neuromuscular Input
- Initiated BFR (blood flow restriction) training for deltoid and scapular stabilizers.
- Manual isometrics with high reps/low load.
- Introduced exercise in the pool focusing on shoulder range of motion.
Week 3-4: Sensorimotor Integration
- Shift to general, functional patterns.
- Incorporation of closed chain scapular patterns.
- Support from a physical therapist to address soft tissue restrictions.
Week 5-6: Functional Loading
- Integrating light push/pull/carry patterns.
- Continued BFR for a “top off” at the end of sessions.
- Intro to plyometrics and medicine ball activities.
Week 7+: Progressive performance
- Continue to increase volume and intensity.
- Advanced plyometrics for upper extremity.
- Advanced throwing and medicine ball activities.
Reflections from a Physical Therapist
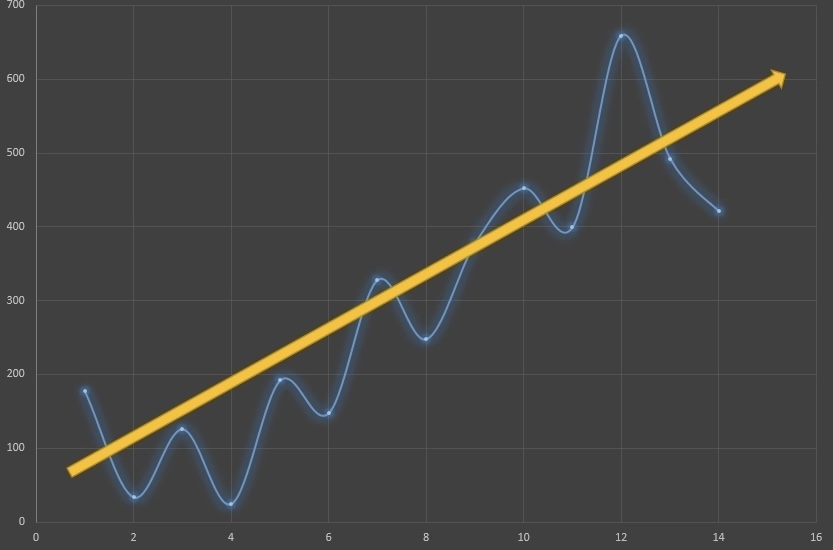
Managing my own injury reminded me that rehab is not linear. I underestimated the psychological load of not being able to train, sleep comfortably, or lift simple objects. Being 2 weeks out I still cannot hold by 2 year old son.
My experience validated the emphasis I place on early acute care modalities, manual therapy, and progressive loading. Recovery is not just about bringing strength and range of motion back; it’s about restoring trust in the joint and the system.
references
- F. Saade et al. “Acromioclavicular joint separation: retrospective study of nonoperative and surgical treatment in 38 patients with grade III or higher injuries and a minimum follow-up of 1 year..” Orthopaedics & traumatology, surgery & research : OTSR (2022): 103405 . https://doi.org/10.1016/j.otsr.2022.103405.
- G. Tang et al. “Comparison of surgical and conservative treatment of Rockwood type-III acromioclavicular dislocation.” Medicine, 97 (2018). https://doi.org/10.1097/MD.0000000000009690.
- Sonnier, J., Kemler, B., Floyd, K., Connors, G., Sabitsky, M., Tjoumakaris, F., Freedman, K., & Paul, R. (2023). Paper 59: No Difference in Post-Operative Outcomes for High-Grade Acromioclavicular Joint Surgery Performed Acutely vs Chronically. Orthopaedic Journal of Sports Medicine, 11. https://doi.org/10.1177/2325967123S00084.
- Sonnier, J., Kemler, B., Coladonato, C., Paul, R., Tjoumakaris, F., & Freedman, K. (2022). Surgical management of acute, high-grade acromioclavicular joint separations: a systematic review. JSES Reviews, Reports, and Techniques, 3, 10 – 20. https://doi.org/10.1016/j.xrrt.2022.10.002.
- L. Bianco Prevot et al. “Surgical vs conservative: what is the best treatment of acute Rockwood III acromioclavicular joint dislocation? A systematic review and meta-analysis.” EFORT Open Reviews, 10 (2025). https://doi.org/10.1530/EOR-2024-0077.


