Approximate Read Time: 10 minutes
“When you understand injury timelines, you better understand what the speed limit is, which routes are possible, and what the potential road blocks may be.”
What You will learn
- Each tissue type—muscle, tendon, ligament, bone, cartilage, nerve—has unique biology influencing how it heals.
- Blood supply is a primary driver of healing capacity, along with cellular specialization.
- Muscle and bone heal relatively quickly; cartilage and nerve are much slower.
- Classifications like Munich and British Athletics guide muscle injury prognosis and communication.
- Understanding biology informs rehab timelines, progression, and communication with athletes and stakeholders.
Biology Is the Blueprint for Injury Timelines
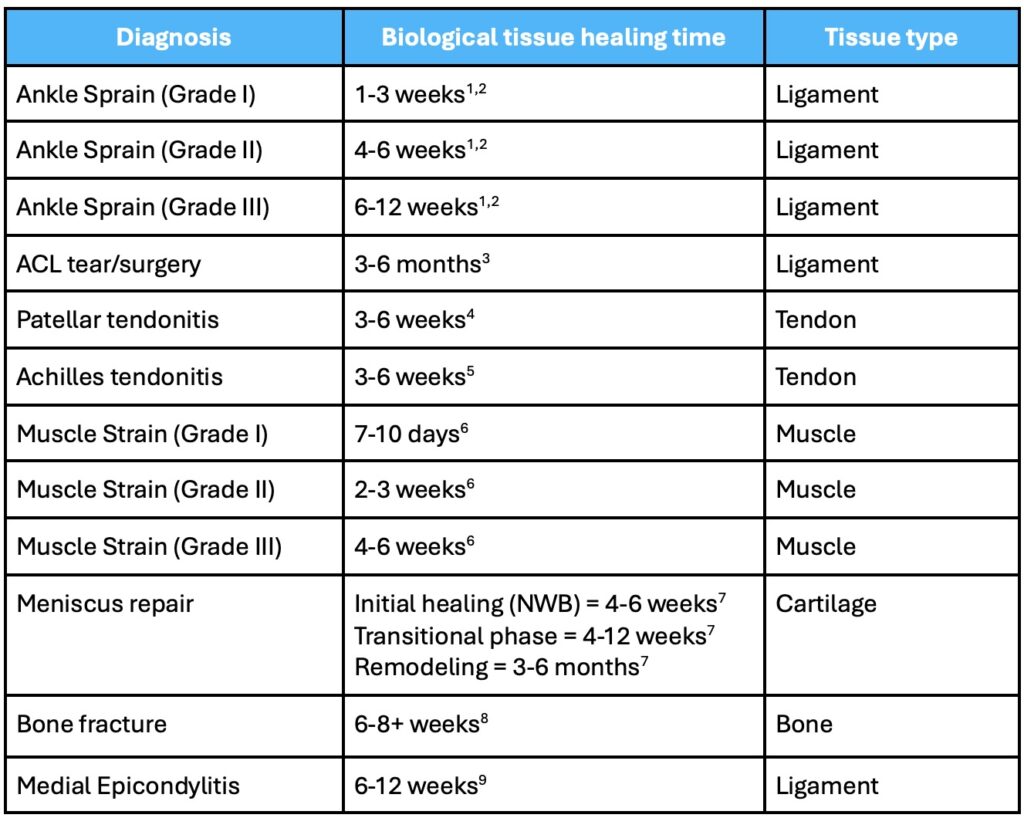
In performance rehab, timelines matter—but only when they’re rooted in physiology. When an athlete asks, “How long until I can play?” the answer shouldn’t just come from a protocol or gut feeling. It should come from an understanding of what the injured tissue is made of, and how it heals.
This article breaks down the cellular composition and vascularity of major musculoskeletal tissues and explores how these properties shape our approach to rehab, programming, and return-to-play expectations.
Muscle Tissue: Richly Vascular, Rapidly Reactive
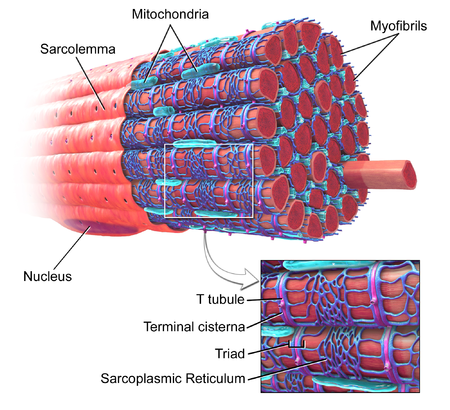
Muscle is one of the fastest-healing tissues in the body thanks to its high blood supply and robust cellular machinery. Muscle fibers (myocytes) contain contractile proteins and are supported by satellite cells that regenerate damaged fibers.
- Mild strain (Grade I): 7–10 days
- Moderate to severe (Grade II–III): several weeks to months
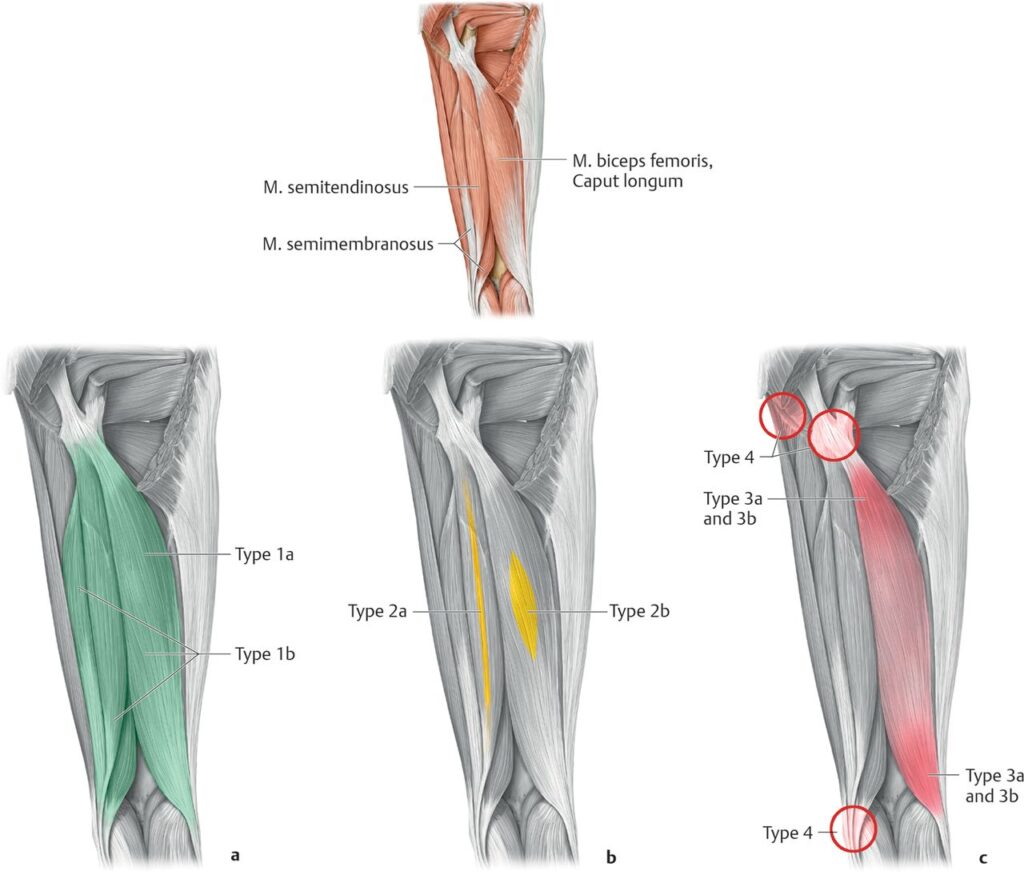
Classification Systems
- Munich Consensus: Differentiates functional vs. structural muscle disorders
- British Athletics: Uses MRI grading (0–4, with a/b/c subclasses) based on location, size, and tendon involvement
These systems help refine prognosis and avoid re-injury—particularly in elite sport where accuracy matters.
Tendon Tissue: Tough, Slow, and Stubborn
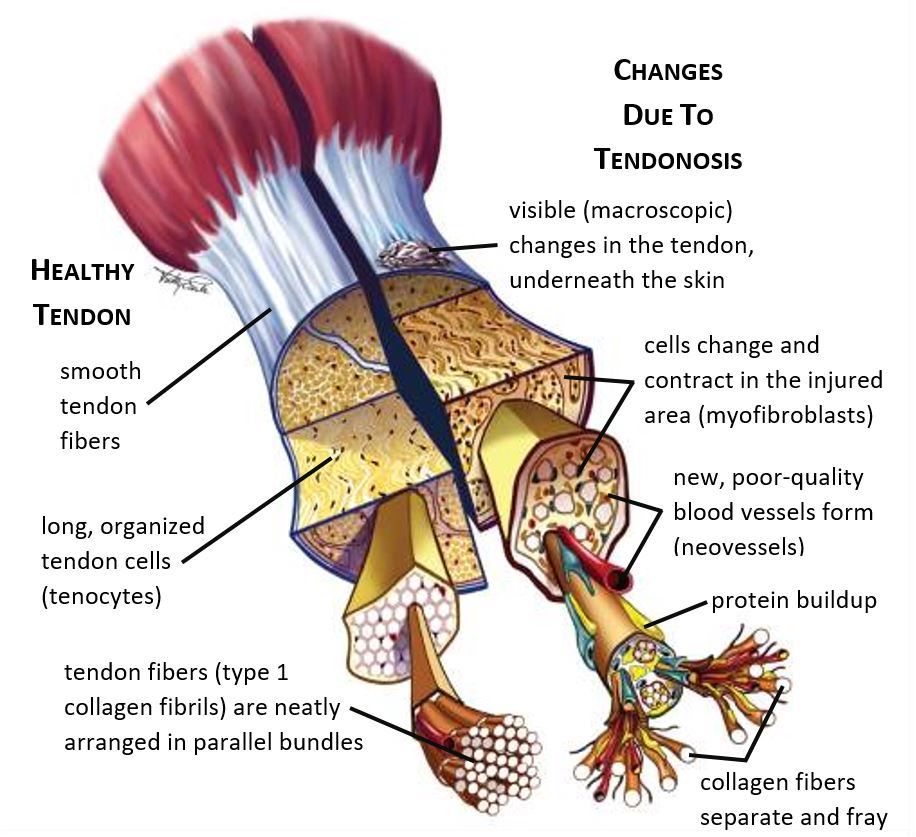
Tendons are dense connective tissues rich in collagen and built to transmit force. But with low vascularity and a lower metabolic rate, they heal slowly.
- Minor tendinopathies: 3–6 weeks
- Chronic or ruptured tendons: months, often surgical
The problem with tendons isn’t just lack of blood—it’s degeneration over inflammation. Rehab needs to emphasize eccentric loading, blood flow stimulation, and patience.
Ligament Tissue: Stability at a Cost
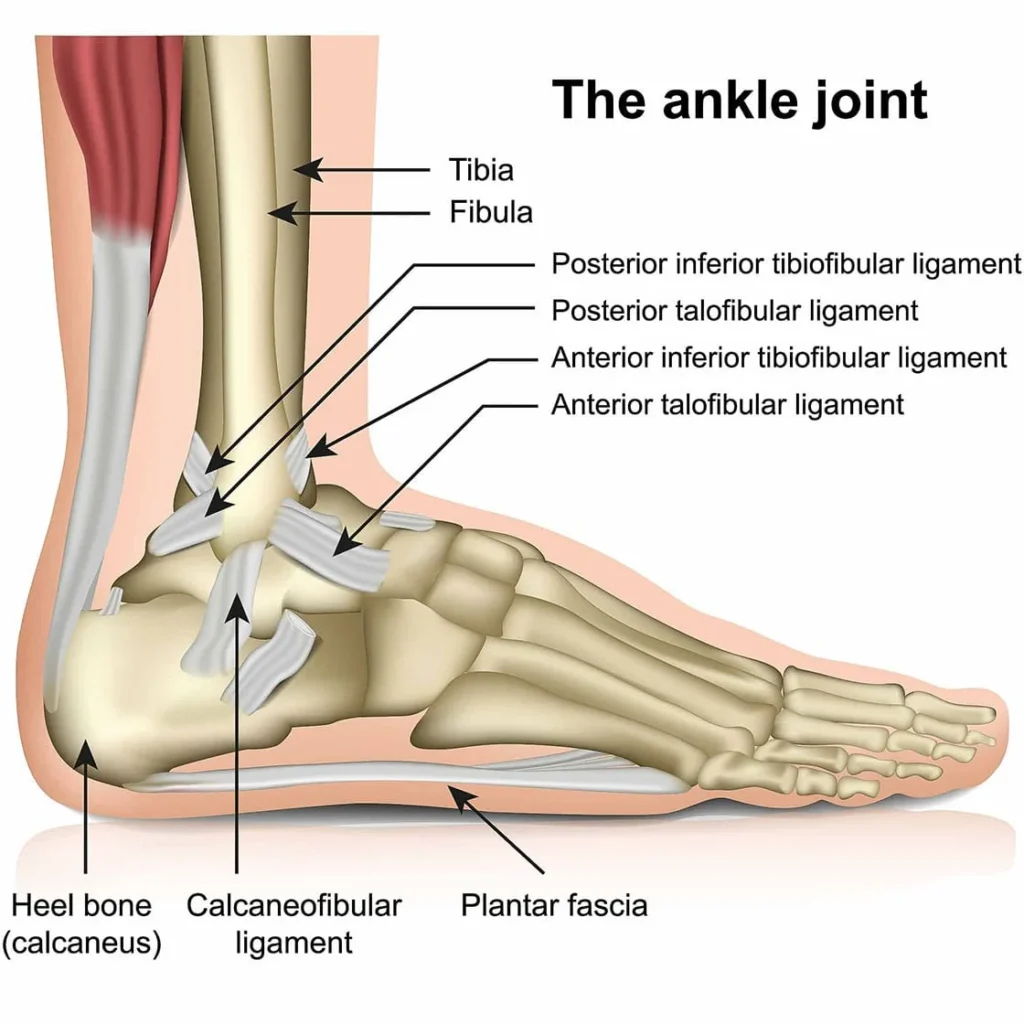
Ligaments resemble tendons structurally but are even more poorly vascularized. Their collagen is less linear and more elastic, allowing for multidirectional joint stability.
- Mild sprains: 1–3 weeks
- Grade II–III sprains or ruptures: 6–12+ weeks
Ligaments are slow to heal and frequently require surgical repair depending on the joint. Expect extended timelines and high recurrence risk without progressive reloading.
Bone: Built to Break—and Rebuild
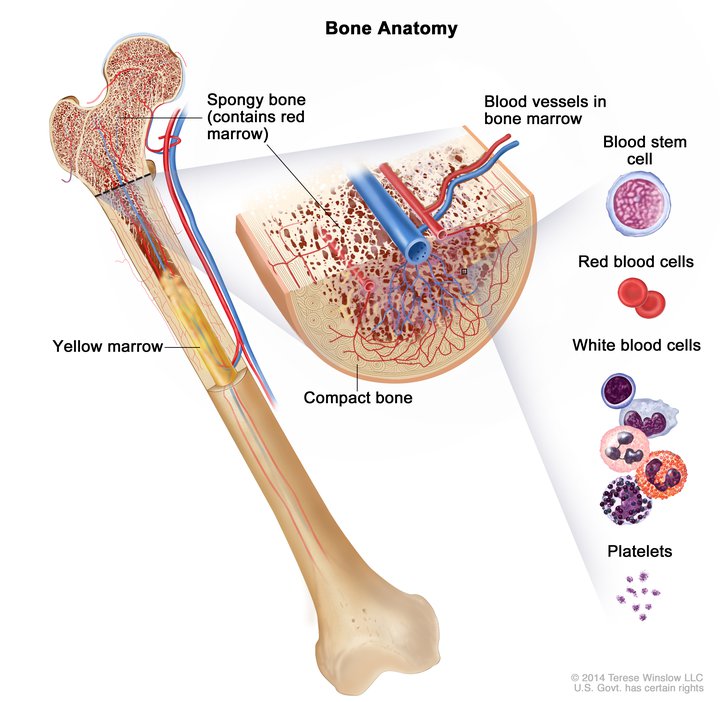
Unlike soft tissue, bone is incredibly vascular and regenerative. It contains osteoblasts and osteoclasts in a dynamic balance of breakdown and rebuilding.
- Simple fractures: 6–8 weeks
- Complex or load-bearing fractures: 12+ weeks
Bone responds well to mechanical stress. Return-to-play should still be governed by imaging and symptom-free loading, not just the calendar.
Hyaline Cartilage: Frictionless, Bloodless, and Fragile
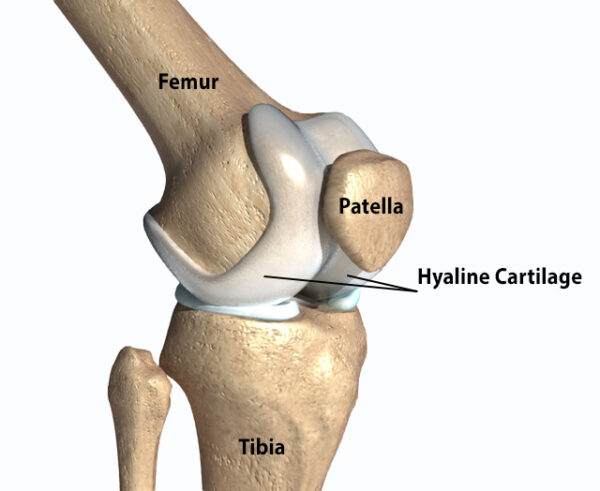
Found at joint surfaces, hyaline cartilage is smooth, frictionless—and terrible at healing. It lacks blood vessels and regenerative cells. Damage to cartilage, especially in the knee or shoulder, often requires surgical intervention.
- Non-operative recovery: limited to none
- Post-op (microfracture or grafts): 3–6 months minimum
Fibrocartilage: Meniscus, Discs, and Healing Zones
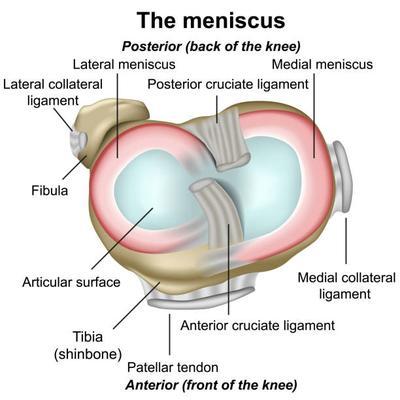
Fibrocartilage blends tensile strength and durability. It appears in the knee meniscus, intervertebral discs, and the wrist’s TFCC. Like hyaline cartilage, it’s poorly vascularized.
- Peripheral zone (vascular): moderate healing
- Central zone (avascular): limited healing; often surgical
Meniscal repairs follow different protocols based on tear location—so don’t assume one-size-fits-all.
Nerve Tissue: Regenerative… But Only Just
Peripheral nerves can regenerate, albeit slowly. Central nervous system nerves (e.g., spinal cord) generally cannot. Schwann cells assist in regrowth, but the timeline is slow:
- Peripheral nerve healing: ~1 mm/day
- Spinal cord injuries: rarely regenerate
Emerging research, particularly in stem cell therapy, is exploring ways to improve nerve recovery. But currently, it remains one of the slowest and most uncertain healing processes in rehab.
What Drives Healing Speed?
Two major factors are going to impact healing speed:
- Blood supply – More blood = faster delivery of nutrients, oxygen, and signaling molecules
- Cellular precursors – Regenerative cells like satellite cells (muscle) or osteoblasts (bone) enable tissue replacement
Tissues with poor blood supply and no regenerative cells—like hyaline cartilage—heal the slowest. Understanding this can help you guide athletes, families, and coaches through realistic expectations.
“Healing isn’t random—it’s predictable, when you understand the biology.”
Final Thoughts: Science as a Storytelling Tool
Knowing the healing profiles of different tissues isn’t just for your own planning—it’s how you build trust. When you can explain why rehab takes time and how tissues recover, you become a better communicator, a better collaborator, and a better clinician.
Progressions make more sense. Timelines become more collaborative. And return-to-play becomes a conversation—not a guess.
References
1) Maughan KL. “Acute Ankle Sprain: An Update,” American Family Physician (Nov. 15, 2006), Vol. 74, No. 10, pp. 1714–20.
2) Martin et al. Ankle Stability and Movement Coordination Impairments: Ankle Ligament Sprains. Journal of Orthopaedic & Sports Physical Therapy, 2013 Volume:43 Issue:9 Pages:A1–A40 DOI: 10.2519/jospt.2013.0305
3) Adams et al. Current Concepts for Anterior Cruciate Ligament Reconstruction: A Criterion-Based Rehabilitation Progression. Journal of Orthopaedic & Sports Physical Therapy, 2012 Volume:42 Issue:7 Pages:601–614 DOI: 10.2519/jospt.2012.3871
4) Maffulli N.et al. Types and Epidemiology of Tendonopathy. Clinical Sports Med. 2003;22 (4):675-92
5) Carcia et al. Achilles pain, stiffness, and muscle power deficits: Achilles Tendonitis. Journal of Orthopaedic & Sports Physical Therapy. 2010:40(9):A1-A26
6) Fernandes TL, Pedrinelli A, Hernandez AJ. MUSCLE INJURY – PHYSIOPATHOLOGY, DIAGNOSIS, TREATMENT AND CLINICAL PRESENTATION. Rev Bras Ortop. 2015;46(3):247–255. Published 2015 Dec 8. doi:10.1016/S2255-4971(15)30190-7
7) Reinold et al. Current Concepts in Rehabilitation Following articular cartilage repair procedures in the knee. Journal of Orthopaedic & Sports Physical Therapy. 2006. 36: 744-794
8) Marsell R, Einhorn TA. The biology of fracture healing. Injury. 2011;42(6):551–555. doi:10.1016/j.injury.2011.03.031
9) Amin et al. Medial Epicondylitis: Evaluation and Management. Journal of the American Academy of Orthopaedic Surgeons: June 2015 – Volume 23 – Issue 6 – p 348–355



