Approximate read time: 25 minutes
The future of tendon rehab isn’t magic—it’s measured. Orthobiologics, movement, and load are no longer separate—they’re synergistic.
What You will learn
- Understand the Continuum Model and why structure, pain, and function don’t always align in tendinopathy.
- Learn how to apply progressive loading—from isometrics to plyometrics—to rebuild tendon capacity.
- Explore the role of motor control and neuroplasticity in tendon pain and rehab success.
- Discover practical load management strategies to guide return-to-play and prevent reinjury.
- Get introduced to emerging biologic treatments like stem cells, exosomes, and peptides as future adjuncts to rehab.
Understanding Tendinopathy and the Continuum Model
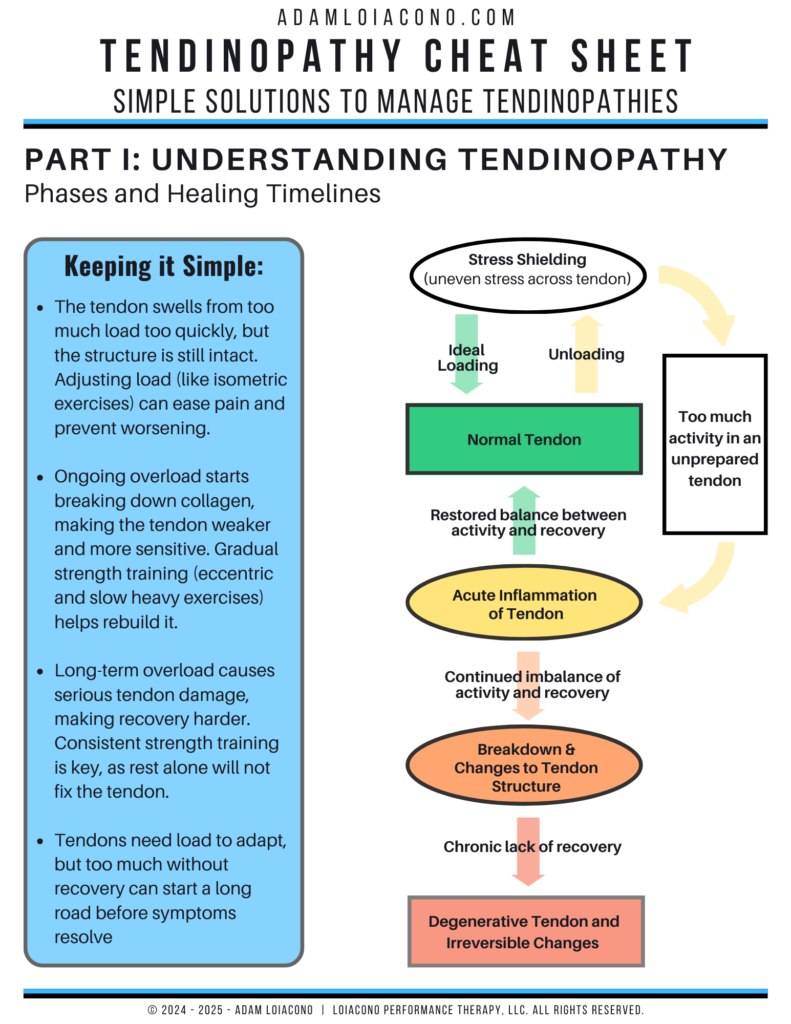
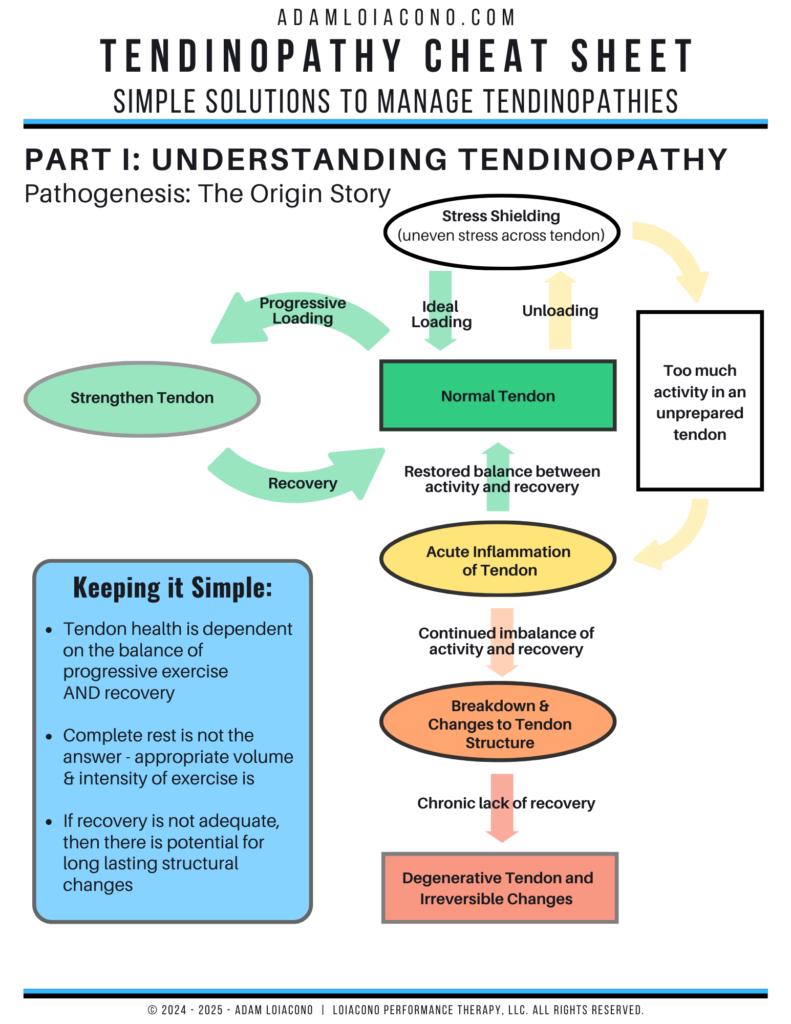
Tendon rehab is not simply a story of “too much load” or “too little rest.” It’s a tale of miscommunication between biological tissue and mechanical demand. Tendons—designed to be robust force transmitters—respond to load through adaptation. But when this adaptation process falters, what emerges is pain, dysfunction, and disorganization of structure.
In the same way a car’s suspension system can wear unevenly from repeated stress, tendons—especially when overloaded, under-recovered, or poorly conditioned—can accumulate structural changes. But here’s the twist: these structural changes do not always predict pain or performance. So if structure isn’t the full story, what is?
This is where the Continuum Model of tendinopathy becomes a vital lens through which we can assess both the pathology and potential for rehab.
The Continuum Model: Moving Beyond One-Size-Fits-All
Originally proposed by Cook and Purdam in 2009 and revisited in 2016, the Continuum Model suggests that tendon pathology progresses through a spectrum of states rather than fitting into a binary “healthy or not” diagnosis.
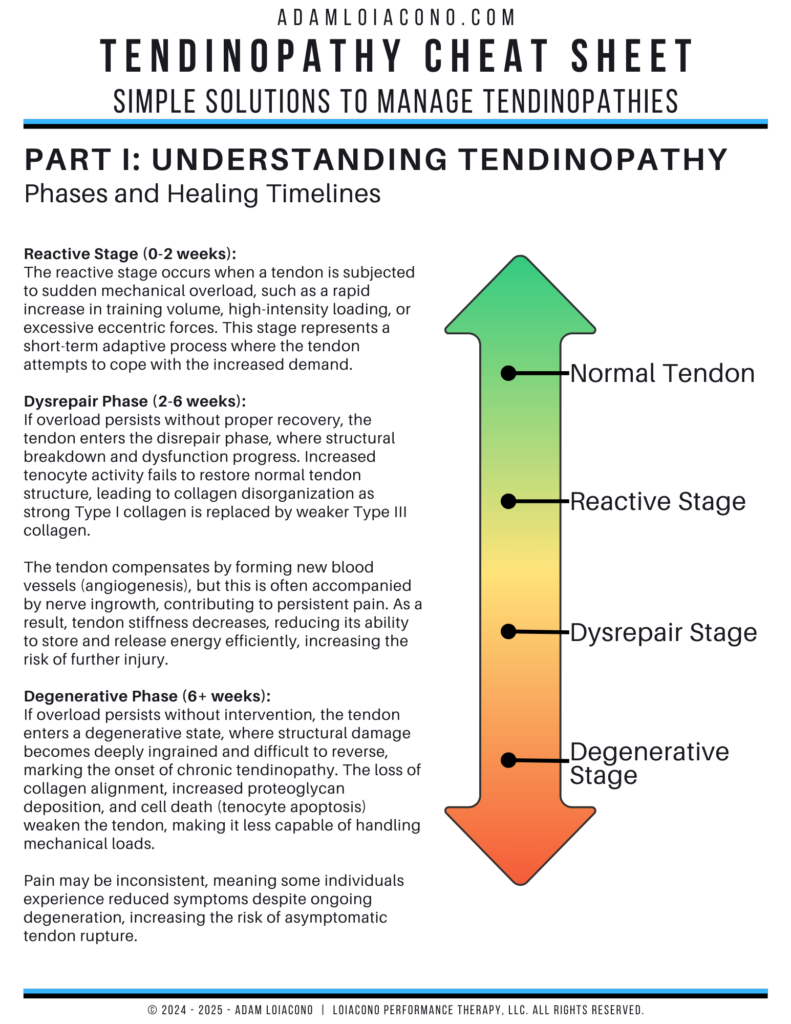
The model outlines three stages:
- Reactive Tendinopathy – A short-term adaptation to acute overload. The tendon responds by swelling and increasing proteoglycan content—leading to increased stiffness and tendon thickness. Think of this as the tendon shouting: “I’m overloaded. Let me protect myself!”
- Tendon Dysrepair – The tendon begins structural disorganization. There is increased cellular activity and matrix breakdown, but some ability to remodel remains. This is the tendon murmuring: “I’m trying to fix things, but I’m struggling.”
- Degenerative Tendinopathy – Extensive disorganization, vascular ingrowth, and reduced capacity to transmit force. This is the tendon going silent—“I’ve adapted poorly, and now I’ve checked out.”
A crucial evolution of the model is the acknowledgment that a single tendon may house multiple stages at once—like a fruit with a bruised spot. For example, a patellar tendon may be degenerative in one region and reactive in another, especially during high-load training.
(if you’re a physical therapist or athletic trainer, I encourage to check out this video with subject-matter expert and research, Jill Cook)
Structure ≠ Pain ≠ Function
One of the central questions since the inception of the Continuum Model is: Does structural pathology cause pain and dysfunction?
The answer: not always.
- Many tendons that show degenerative changes on ultrasound or MRI are pain-free.
- Conversely, patients with no visible pathology can have severe tendon pain.
- Structural improvement following rehab doesn’t always correlate with pain relief or performance improvement.
In other words, structure, pain, and function are interrelated—but not directly proportional. This complexity makes treatment challenging, especially when patients (or clinicians) focus solely on imaging findings.
Think of a tendon like a suspension bridge. You can have some worn cables (degenerative fibers) and still safely drive across it if the rest of the bridge (aligned fibrillar tissue) is strong and stable. Our job is to reinforce what’s strong and reduce stress on what’s not.
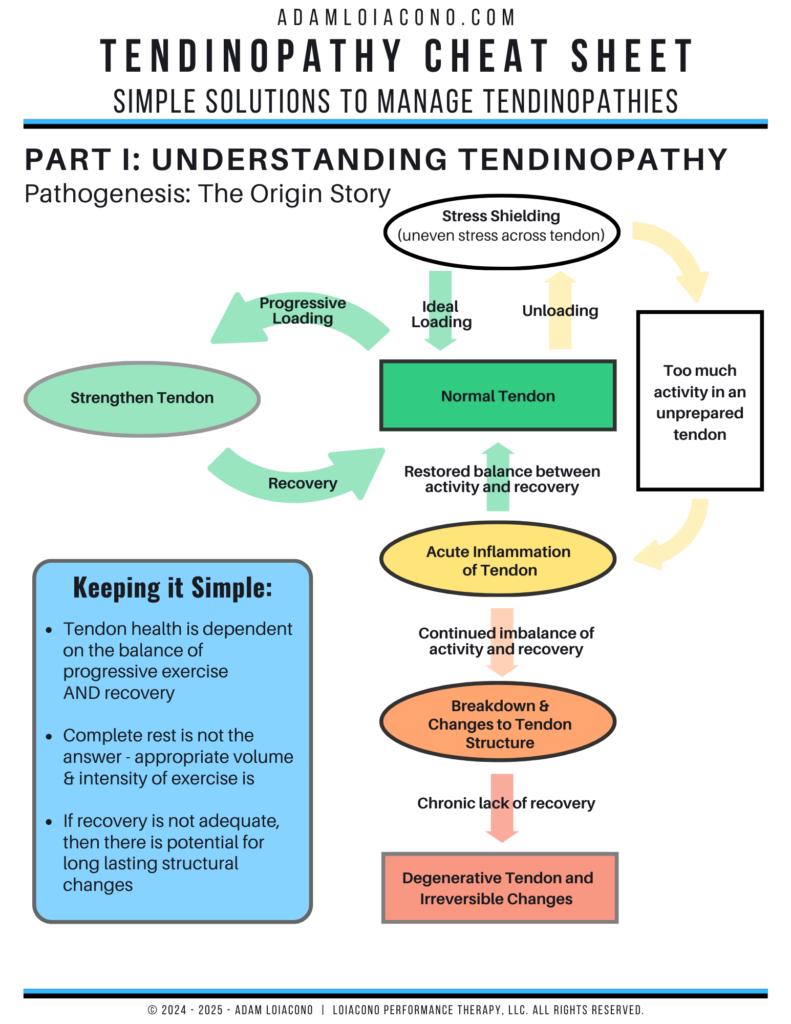
The Role of Load in Tendon Health: Friend and Foe
Tendons are mechanosensitive. Load is both the cause and the cure. When load is:
- Appropriate → Tendons adapt by increasing stiffness, collagen synthesis, and energy efficiency.
- Too much, too soon → The result can be reactive tendinopathy.
- Absent or inadequate → The tendon weakens, losing capacity and risking pathology from normal tasks.
This brings us to an essential point from Docking & Cook’s 2019 review: adaptation is about more than just tissue change—it’s about person-level function. While ultrasound and MRI can show response to load, they don’t tell us how an athlete performs or tolerates volume over time. The goal of high-performance rehab must be to restore both tendon structure and athletic capacity.
The Imaging Dilemma: Seeing Isn’t Always Believing
Advanced imaging can reveal thickening, Doppler signals, and collagen disarray. But these findings are not always indicative of pain or function. Up to 80% of tendons with abnormal imaging remain asymptomatic, and imaging cannot reliably predict recovery or response to intervention.
“Structure doesn’t matter until it matters.” – Bill Hartman (human performance expert, mentor, and above all else a close friend)
Think of a rope. If you inspect a rope and see fraying on one side, that doesn’t necessarily mean the rope will snap. Its load-bearing capacity may still be intact. Clinically, this means:
- We cannot rely on imaging alone to guide rehab decisions.
- Language used to describe imaging matters. Using terms like “tear” or “degeneration” may catastrophize the condition and reduce patient confidence, leading to poorer outcomes.
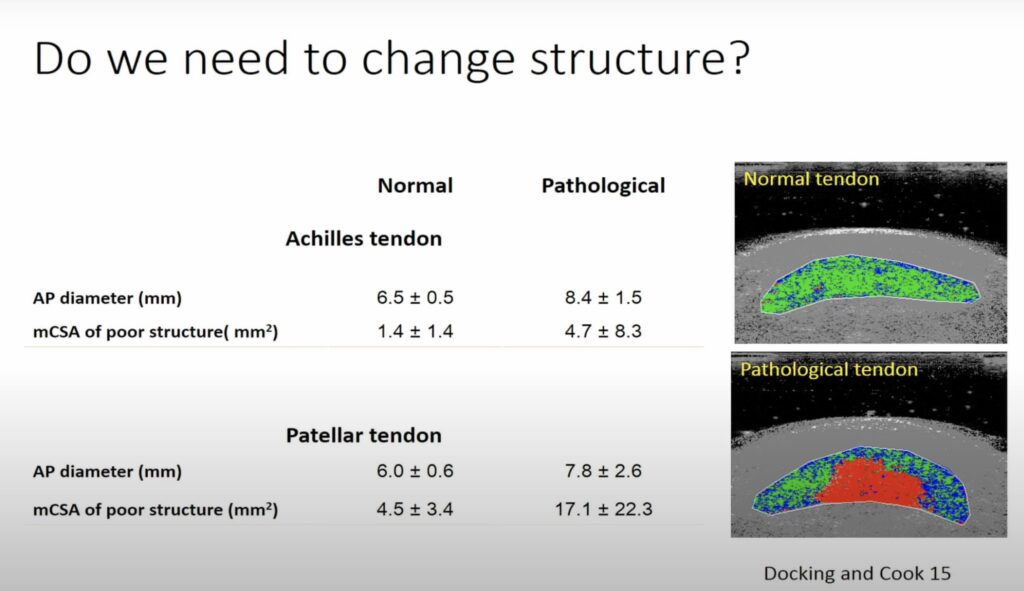
This image above shows the normal pathology of the tendinopathy, and highlights the thickening of the healthy portion of the tendon to compensate for the pathological portion. Imaging like this begs the question should we be concerned about thick tendons, or are they simply a reflection of necessary adaptations born out of pathology?
Neuromotor Considerations: Beyond the Tendon Itself
Tendinopathy affects not just the tendon but the entire neuromuscular system. Research by Ebonie Rio et al. shows changes in corticospinal drive, motor inhibition, and even bilateral motor adaptations, suggesting that tendon pain leads to altered motor control—sometimes system-wide.
- Athletes with patellar tendinopathy demonstrate increased cortical inhibition and excitability, even on the contralateral side.
- Motor control strategies often remain altered even after symptoms resolve, potentially contributing to recurrence.
The nervous system during a tendinopathy is like a software update gone wrong. The brain tries to “protect” the tendon by altering muscle activation patterns, but this protection may persist even after the pain is gone, creating a mismatch between intention and movement.
Summary: The Diagnostic and Clinical Challenge
The “problem” in high-performance tendon rehab is not a simple equation of pain = injury = rest. Instead, we must navigate:
- Structural changes that may or may not matter.
- Pain that may be locally driven, centrally influenced, or both.
- Functional deficits that linger even after symptoms fade.
- A need for person-centered rehab that builds load capacity, not just symptom relief.
This demands a thoughtful approach that incorporates imaging (without overemphasizing it), respects the role of the central nervous system, and uses mechanical loading to build resilience.
In the next section, we’ll shift from problem to solution—covering the evidence-based progression from isometrics to plyometrics, how load management strategies optimize tendon health, and the rationale behind procedures like Tenex.
100% Free Access
Take Control of Your Performance and Stay Injury-Free
Discover the 5 powerful tools of the proven 3P Injury Prevention Toolkit + receive weekly emails that will help you improve performance and live pain free (and the latest podcast news)
Current Strategies to Restore Tendon Function and Performance
Now that we’ve outlined the complexity of tendinopathy, including the inconsistencies between pain, structure, and function, the natural next question becomes: What do we do about it?
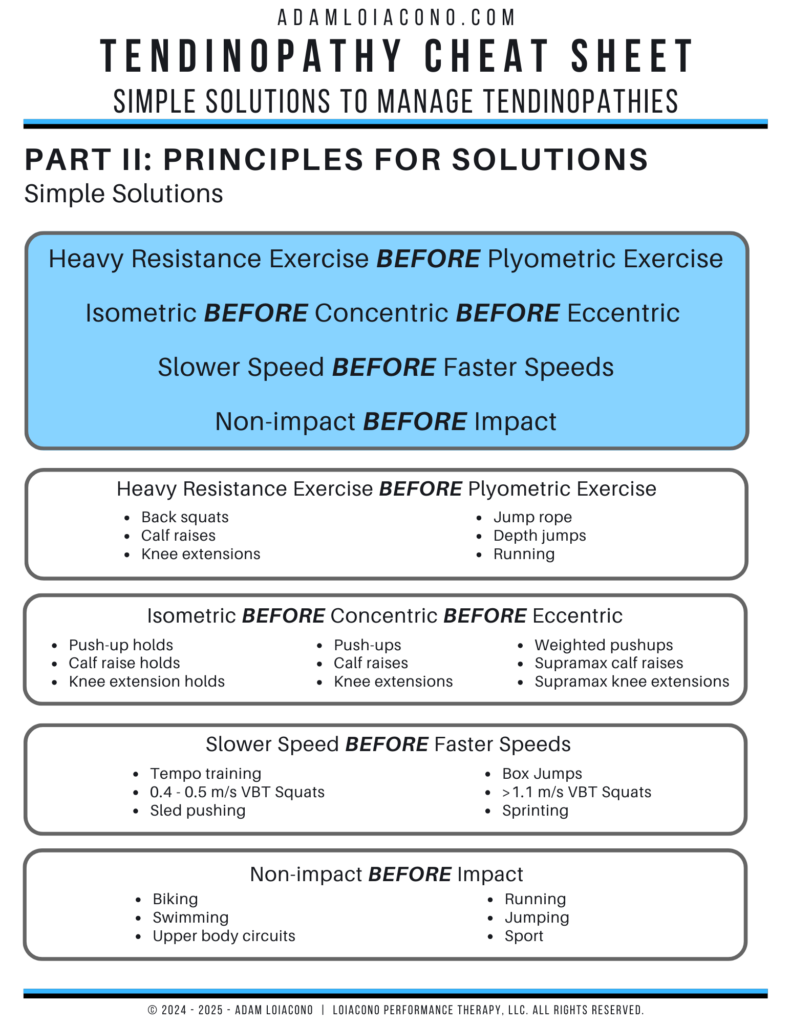
While the pathophysiology of tendinopathy may feel like navigating a maze, the way out isn’t as mysterious as it once was. Over the past two decades, we’ve seen a strong consensus emerge: progressive mechanical loading is the most reliable, non-invasive tool we have. When executed with intent, loading not only addresses tissue health but also motor control, performance capacity, and athlete confidence.
Isometrics: The “Reboot Button” for Painful Tendons
When tendon pain is high—especially during activities of daily living or sport—our first step isn’t to avoid loading. It’s to modulate loading. Enter isometrics, a powerful starting point.
Isometric exercises are static muscle contractions held at a joint angle without movement. They were reintroduced into tendon rehab by Rio et al. for their dual benefits:
- Immediate pain relief (via cortical inhibition modulation).
- Low mechanical strain on the tendon, making them safe during painful flares.
Isometrics as a dimmer switch. They lower the intensity of pain signals without completely turning off the lights.
Isometrics allows the athlete to stay engaged in training rather than shutting down. The strength & conditioning is well versed in the benefit of isometric activity for developing speed and power. We can apply similar principles with less load to help re-introduce activity while mitigating pain, here is how:
- 5 sets of 45-second holds at 70% maximum voluntary contraction.
- Movements should mimic sport-specific joint angles (e.g., knee flexion angle in jumpers).
But as helpful as they are, isometrics are not curative. They address the “software”—the pain system and motor inhibition—but we still need to upgrade the “hardware.”
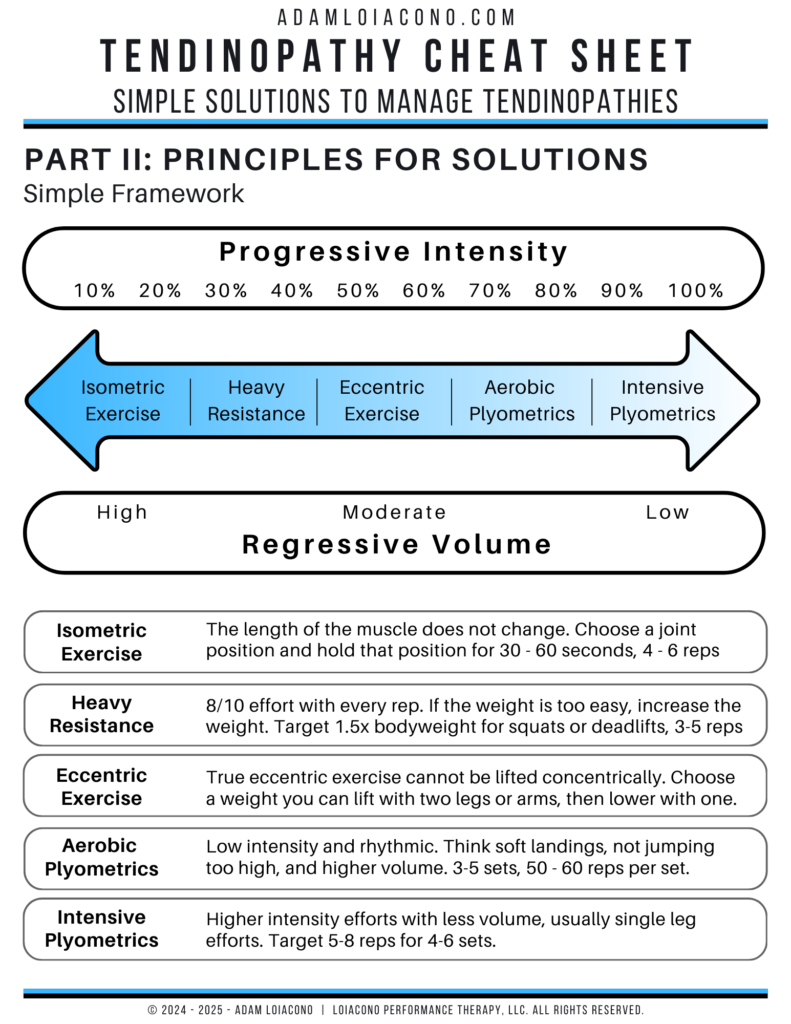
Heavy Resistance Training: The Foundation of Tendon Remodeling
Once pain is manageable, the next step is progressive resistance training. Tendons thrive under tension—but they’re slow adapters. Unlike muscle, which hypertrophies relatively quickly, tendon collagen turnover is glacial in pace. That’s why consistency and progression matter more than novelty.
The most frustrating thing about a tendinopathy is symptoms often come on slowly, and they equally are slow to recover.
There are two primary methods of tendon-loading strength work:
- Heavy Slow Resistance (HSR) Training
- Slow, controlled reps (3–5 seconds per phase) at moderate-to-heavy loads.
- Combines eccentric and concentric loading.
- Shown to be more effective than eccentrics alone in improving function and pain in Achilles and patellar tendinopathy.
- Target goal should be 1.0x bodyweight on calf raises and knee extension OR 1.5x for squatting activities
- Eccentric-Only Training
- Use of calf raises + heel drops for Achilles; decline squats for patellar.
- Still effective, especially when concentric loading is provocative.
- May promote greater tendon stiffness, but lacks the strength gains of HSR.
If tendinopathy is like potholes forming on a frequently traveled road, HSR and eccentric training act like repaving crews—gradually reinforcing the surface through repeated, targeted stress.
Programming Principles:
- Begin with 3–4 sets of 8–10 reps at 70–85% 1RM.
- Emphasize time under tension.
- Progress over 4-8 weeks.
- Prioritize unilateral loading when asymmetry exists.
Neuromotor Considerations:
According to Rio et al., strength work that’s externally paced—using a metronome or visual cue—can optimize corticospinal drive and reduce motor inhibition. This strategy, called Tendon Neuroplastic Training (TNT), addresses both mechanical and neurological dysfunctions.
Plyometrics: Teaching the Tendon to Store and Release Energy
A healthy tendon is a spring. It stores energy during deceleration and releases it during propulsion. Strength work loads the tissue. Plyometric work teaches it to release.
Once an athlete can tolerate heavy loading and has adequate strength (e.g., single-leg squat ≥ bodyweight, pain-free hop tests), it’s time to add rate-dependent stimuli:
- Jumping
- Hopping
- Bounding
- Depth drops
If strength training is like building the car’s engine, plyometrics are the suspension system—tuning for speed, responsiveness, and resilience
Here is a simple progression for plyometrics:
- Sub-maximal Rebounds (low amplitude, focus on rhythm).
- Single-leg Hops (introduces asymmetrical force).
- Bounding & Change of Direction (lateral and transverse vectors).
- Depth Drops & Landings (eccentric rate of force development).
- Sport-specific Drills (closed → open chain, predictable → reactive).
Plyometrics reintroduce stretch-shortening cycle demand, which is essential for athletes in jumping, sprinting, or change-of-direction sports. Exercise and rehab for tendons must get to this stage, but we must introduce gradually, monitor pain response, and de-load if needed. Reassess functional tasks weekly using hop tests or force plate metrics if available.
Load Management: Navigating the Return-to-Play Highway
You can do all the right exercises—but if the load profile of the athlete exceeds the tissue’s capacity, setbacks will follow. This is where load management strategies come into play.
Tendon rehab isn’t just about what happens in the weight room—it’s about how those adaptations are layered into weekly workloads. The concept of the Acute:Chronic Workload Ratio (ACWR) can help here:
- Acute load: the most recent 7-day volume or intensity.
- Chronic load: the rolling 28-day average.
Maintaining a 1.0–1.3 ratio (i.e., not ramping up too quickly) has been shown to reduce injury risk in several sports. More simply put, maintain incremental increases in volume and intensity week to week and avoid massive drop offs in load to minimize the detraining effect.
Think of chronic load as your tendon’s credit score. If it’s solid, you can “spend” a little more (acute stress). But if your chronic load is poor, even small spikes can bankrupt the system.
The Tenex Procedure: Minimally Invasive Relief for Degenerative Tendons
For a small subset of individuals—especially those with focal tendon degeneration and persistent pain unresponsive to 4–6 months of progressive rehab—a minimally invasive procedure like Tenex may offer a valuable next step.

The Tenex procedure is an ultrasound-guided percutaneous technique that uses high-frequency ultrasonic energy to debride and aspirate degenerative tendon tissue. Rather than cutting open the tendon surgically, Tenex creates a small incision (typically 3–5 mm) and uses a specialized probe to precisely remove only the disorganized, non-viable tissue.
Indications for Tenex include:
- Focal tendinopathic lesions with failed conservative care.
- Persistent symptoms localized to one region of the tendon.
- Common sites: proximal hamstring, patellar tendon, Achilles tendon, and common extensor tendon at the elbow (e.g., lateral epicondylitis).
Why It Works:
- Degenerative tendon regions often lack appropriate load transmission and are “mechanically silent.”
- By removing these non-functional areas, Tenex can relieve local nociceptive drivers while preserving the surrounding healthy tissue.
Think of the tendon like a rope with a few frayed fibers. Tenex trims the frays so the rest of the rope can function more effectively, without completely replacing or reattaching it.
As physical therapists, athletic trainers, or strength and conditioning coaches, we play a key role in making the most of the post-procedure window. A few key points:
- Surgery removes the “hole,” but now you must rebuild the doughnut. The degenerated tissue is gone, but tendon capacity is not automatically restored.
- Load tolerance still needs to be rebuilt through isometric and progressive resistance loading.
- Post-op progression typically begins with light range of motion and isometrics in the first 1–2 weeks, with a gradual return to HSR by weeks 4–6 and energy-storage activities like plyometrics after 8–12 weeks.
The Tenex procedure is like precision landscaping for the tendon. It removes only the dead weeds while preserving the rest of the garden—but without regular watering and conditioning, the garden won’t thrive. That’s where high-performance rehab fills the gap
Today’s Tendon Rehab Is Smart, Strategic, and Individualized
The “solution” to tendinopathy is not found in a single exercise or protocol—it’s in the principled progression of load, the integration of neuromotor retraining, and the alignment of rehab with sport demands. The strategies outlined above are the gold standard today, but as you’ll read next, new tools are emerging on the horizon—ones that may help us further amplify tendon healing.
In the final section, we’ll explore orthobiologics—including the emerging roles of mesenchymal stem cells (MSCs), exosomes, and peptides as adjuncts to progressive loading and as part of a regenerative toolbox for the modern rehab professional.
| Phase | Focus | Tools/Methods |
|---|---|---|
| Pain Management | Reduce nociception, maintain engagement | Isometrics, TNT, education |
| Tissue Remodeling | Restore load tolerance, build capacity | HSR, eccentrics, externally paced strength |
| Energy Storage | Reinforce tendon’s dynamic function | Plyometrics, jump tests, COD drills |
| Return to Play | Reintegration of full sport demands | ACWR, sport-specific drills, coach coordination |
Orthobiologics and Tendon Rehab
In the world of sports performance and rehabilitation, we’re taught that movement is medicine. But in some cases—particularly when chronic tendon pain persists despite well-executed rehab—we begin looking for new tools to complement the mechanical work. That’s where orthobiologics enter the conversation.
Biologics such as mesenchymal stem cells (MSCs), exosomes, and peptides are emerging as next-generation interventions for tissue healing. While these are not replacements for sound load-based rehabilitation, they may provide a biological nudge to support tendon recovery, especially in difficult cases.
Let’s explore what these tools are, how they work, and how they might support tendon healing in a high-performance model.
Learn from some of Arizona’s top sports doctors, Dr. Chuck Peterson and Dr. Cam Davis, as they share more insights into the world of orthobiologics. Follow the link below to listen to this episode of the Finding Small Wins podcast.
Mesenchymal Stem Cells (MSCs): The Builders and Signalers
MSCs are stem cells capable of differentiating into various tissue types, including tenocytes—the cells responsible for maintaining tendon matrix. But their true power may not lie in what they become, but in what they secrete. Here is how MSCs can help:
- Paracrine signaling (cell communication): MSCs release cytokines and growth factors that reduce inflammation, stimulate repair, and guide tissue regeneration.
- Tenogenic differentiation (to be or not to be tendon cells): Under the right conditions, they can promote the synthesis of collagen type I, helping restore structural integrity.
- Immune modulation (MSCs’ secret weapon): MSCs help downregulate chronic inflammation that contributes to tendon degeneration.
MSCs like a foreman on a construction site. They may not do all the heavy lifting, but they direct traffic, call in reinforcements, and keep the repair process on track.
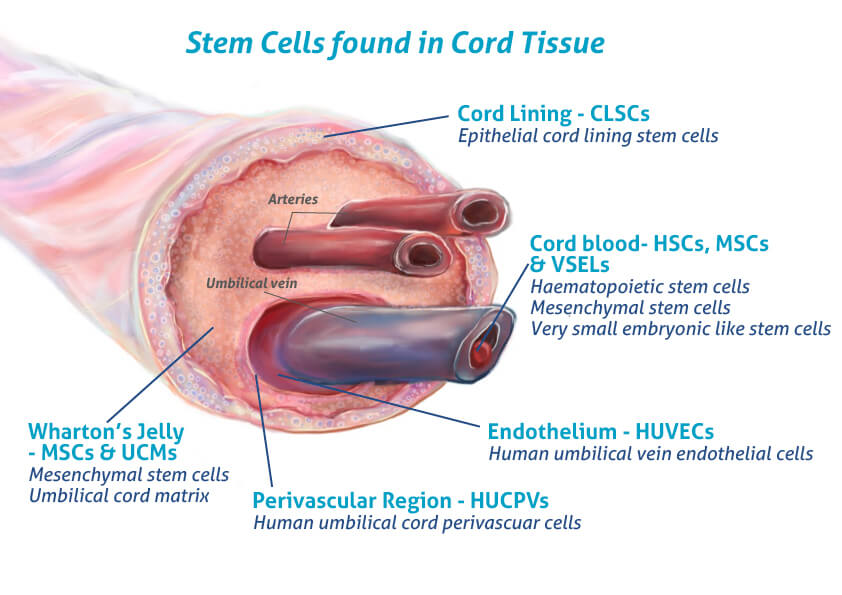
Exosomes: Nature’s Tiny Text Messages
Exosomes are extracellular vesicles—nano-sized bubbles secreted by cells (including MSCs)—that carry proteins, RNA, and lipids to nearby or distant cells. Here is how exosomes can help:
- Exosomes from MSCs can promote tenocyte proliferation, collagen synthesis, and angiogenesis.
- They reduce pro-inflammatory cytokines and inhibit fibrosis, key in controlling chronic tendon disrepair.
- Being acellular, exosomes have a lower risk of immune reaction and are easier to store and transport.
If MSCs are the foremen, exosomes are the text messages they send to subcontractors with exact instructions for repairs.
Peptides: Biological Tweaks to the Repair Process
Peptides are short chains of amino acids that act as messengers in the body. Several naturally occurring and synthetic peptides have been investigated for their ability to support tendon healing. Research is still emerging, but there seems to be growing evidence that peptides like BP-157 can have a role in the healing of tendinopathies.
I have not come across clinical research specifically for BP-157 for tendinopathies, but the research is there supporting how BP-157 can accelerate healing of a variety of musculoskeletal conditions. From my perspective, I’ve yet to see a negative contraindication for the use of peptides, only positive indications. If it can’t hurt, then why now?
If MSCs are the foreman, and exosomes are the text messages to the subcontractors, then peptides are the interior designer – they come in and help fine tune the final structure and bring everything together.
Integrating Biologics Into High-Performance Rehab
The most progressive way to think about orthobiologics is not as a shortcut—but as an adjunct.
- For the reactive tendon: Biologics may not be necessary. Load-based strategies remain primary.
- For the degenerative tendon: Especially when pain persists after 3–6 months of structured loading, biologics may offer a biological reset and promote the growth of health tissue.
- For post-operative healing: MSCs and exosomes may enhance surgical outcomes by stimulating early matrix remodeling and reducing scar formation.
| Stage | Primary Focus | Biologic Adjunct |
|---|---|---|
| Painful Reactivity | Load modulation, isometrics | None or education only |
| Early Disrepair | Heavy slow resistance, tempo training | Consider peptides or exosomes |
| Degeneration/Non-responder | Load capacity + biologic reset | MSCs, exosomes, peptides (based on evaluation) |
| Post-op Tenodesis | Restore function + prevent re-injury | MSCs + progressive loading |
Caution: As exciting as these tools are, we must be wary of hype. Most studies are small, and standardization (dosing, delivery, sourcing) is still evolving. Always layer orthobiologics on top of a strong foundation: Principles → Process → Plans.
Conclusion – Merging the Present and Future of Tendon Rehab
We began this article by revisiting the problem—the complexity of tendinopathy. Through the Continuum Model, we learned that tendon structure, pain, and function don’t always correlate, and that treating tendinopathy demands more than just chasing imaging findings.
We then explored the solution—today’s best practices: isometrics to manage pain, heavy resistance training to rebuild capacity, plyometrics to restore performance, and load management to sustain durability. These are not just exercises; they are strategic stress applications aimed at rebuilding a spring, not a sponge.
And now, we’ve explored the future—where science meets innovation. Orthobiologics like MSCs, exosomes, and peptides may soon become valuable adjuncts to rehab, offering a biological assist to help tendons adapt more completely and recover more predictably.
But the core message remains this: There is no replacement for sound programming, thoughtful progression, and individualized care. Tendon rehab isn’t just about fixing a tissue—it’s about upgrading a human.

insightful videos
Subscribe today to Adam’s YouTube channel to get the latest on rehab, training, sports science, and so much more!
References
- Cook JL, Rio E, Purdam CR, Docking SI. Revisiting the continuum model of tendon pathology: what is its merit in clinical practice and research? Br J Sports Med. 2016;50(19):1187-1191. doi:10.1136/bjsports-2015-095422
- Rio E, Kidgell D, Moseley GL, et al. Tendon neuroplastic training: changing the way we think about tendon rehabilitation. Br J Sports Med. 2016;50(4):209-215. doi:10.1136/bjsports-2015-095215
- Docking SI, Cook JL. How do tendons adapt? Going beyond tissue responses to understand positive adaptation and pathology development: A narrative review. J Musculoskelet Neuronal Interact. 2019;19(3):300-310.
- Docking SI, Cook JL. Imaging and its role in tendinopathy: current evidence and the need for guidelines. Curr Radiol Rep. 2018;6:43. doi:10.1007/s40134-018-0302-8
- Sharma P, Maffulli N. Tendon injury and tendinopathy: healing and repair. J Bone Joint Surg Am. 2005;87(1):187-202. doi:10.2106/JBJS.D.01850
- Wang A, Ao Y, Wang H, et al. Stem cell therapy in tendon injuries: a systematic review and meta-analysis of basic science evidence. Cell Transplant. 2016;25(10):1839-1850. doi:10.3727/096368916X692362
- Dakin SG, Martinez FO, Yapp C, et al. Inflammation activation and resolution in human tendon disease. Sci Transl Med. 2015;7(311):311ra173. doi:10.1126/scitranslmed.aac4269
- Gwyer D, Wragg NM, Wilson SL. Gastric pentadecapeptide body protection compound BPC 157 and its role in accelerating musculoskeletal soft tissue healing. Cell Tissue Res. 2019;377(1):153-159. doi:10.1007/s00441-019-03016-8