“Understanding the biochemical and neuromuscular principles of physical touch reduces the noise of which manual therapy techniques are superior to others.”
Adam Loiacono
What You Will Learn
- Endocrine, neural, & mechanical influences from manual therapy.
- Relevant research on manual therapy and biological processes.
- Advice on how to integrate manual therapy with sports rehab.
What Really Happens During Manual Therapy
Manual therapy and exercise are physical therapists’ two largest tools in their toolbox when it comes to sports rehab. Within each of these main tools exists dozens if not hundreds of schools of thought, theory, or techniques that tend to elicit similar outcomes. Similar to my 3P Framework for Return to Play, I believe in guiding principles when it comes to manual therapy. The first step to my principles is staying rooted in the fundamental biological processes that occur when we provide manual therapy. Let’s explore some of the biological processes.
The Endocrine System
Manual therapy, including methods such as massage, mobilization, and manipulation, can elicit a complex endocrine response involving various hormonal changes that can contribute to the therapeutic effects observed.
During manual therapy, the mechanical pressure and movement applied to the body’s tissues may stimulate the nervous system, which in turn can affect the endocrine system. This interaction between the nervous system and endocrine system is essential for maintaining homeostasis and is mediated through neuroendocrine pathways.
Firstly, manual therapy has been associated with the increased release of endorphins, which are endogenous opioids produced by the central nervous system. These hormones act as natural painkillers and induce a sense of well-being. A study by Field et al. (2005) showed that moderate pressure massage led to increased levels of endorphins, suggesting a potential mechanism for the pain-relieving effects of manual therapies.
Secondly, manual therapy may reduce the levels of stress hormones, such as cortisol. Cortisol is a steroid hormone released in response to stress and has various physiological effects, including immune suppression and increased blood glucose. A study by Rapaport et al. (2012) indicated that patients who received regular massage therapy had lower levels of cortisol compared to control subjects, indicating a stress-reducing effect of manual therapy.
Additionally, manual therapy can influence the secretion of oxytocin, a hormone associated with social bonding, relaxation, and stress reduction. Oxytocin is also thought to have anti-inflammatory effects, which may contribute to the therapeutic benefits of manual therapy. A research article by Uvnäs-Moberg et al. (2015) suggests that the pressure exerted during massage can stimulate the release of oxytocin, which may in turn facilitate healing and reduce discomfort.
These hormonal changes are believed to be mediated through pressure receptors under the skin that, when stimulated during manual therapy, send signals to the brain to release various hormones. This can lead to physiological changes that promote relaxation, reduce pain, and enhance tissue healing.
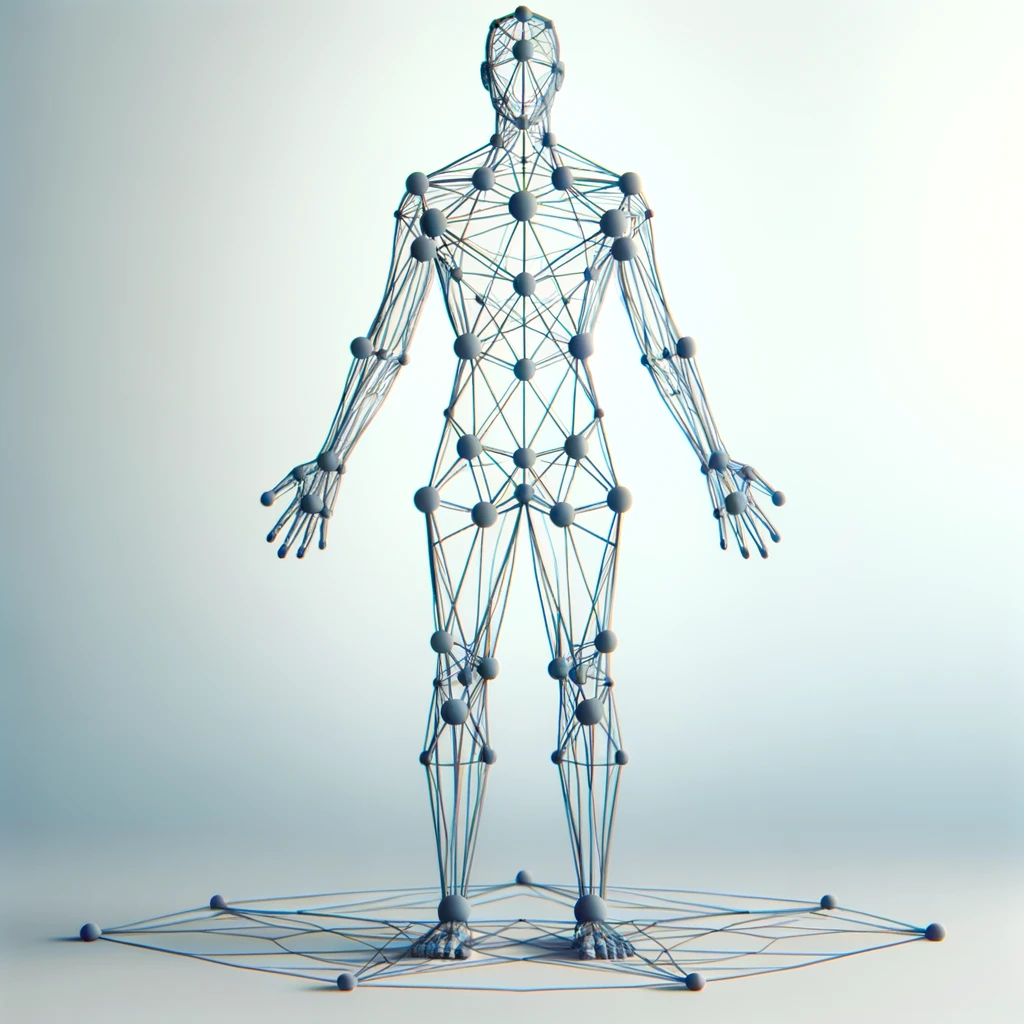
Biotensegrity and Mechanotransduction
Biotensegrity and mechanotransduction are fundamental concepts that underpin the physiological responses associated with manual therapy. These two interconnected scientific principles help to explain how manual manipulation of the body’s tissues can lead to both local and systemic effects, influencing health and healing.
Biotensegrity is a term derived from “biological tensegrity” and describes the architectural principle of structural balance within biological organisms. Tensegrity structures consist of elements that withstand tension, like muscles and tendons, and elements that resist compression, such as bones. This continuous tension and discrete compression create a dynamically stable, three-dimensional structure that distributes mechanical forces throughout the body efficiently. Biotensegrity applies this principle to human anatomy, suggesting that the musculoskeletal system functions as a unified, interconnected network rather than a series of isolated parts. This framework is essential in understanding how forces applied during manual therapy can have far-reaching effects beyond the point of application.
Mechanotransduction refers to the processes by which cells convert mechanical stimulus into chemical activity. It is the means through which cells sense and respond to mechanical signals by initiating cascades of molecular events that can influence cellular behavior, gene expression, and extracellular matrix remodeling. In the context of manual therapy, the application of mechanical forces can lead to changes at the cellular level that affect tissue repair, inflammation, and pain perception.
Mechanoreceptors & Manual Therapy
The interplay between biotensegrity and mechanotransduction during manual therapy can be understood through the lens of the body’s mechanoreceptors, which are sensory receptors that respond to mechanical pressure or distortion. There are several types of mechanoreceptors, including:
- Pacinian corpuscles: Respond to deep pressure and high-frequency vibration.
- Ruffini endings: Detect skin stretch and contribute to the kinesthetic sense of the body and the control of finger position and movement.
- Meissner’s corpuscles: Sensitive to light touch and texture changes.
- Merkel’s disks: Respond to light pressure and provide detail information.
- Free nerve endings: Respond to various stimuli including pressure and noxious stimuli.
During manual therapy, these mechanoreceptors are stimulated by the pressures and movements applied by the therapist. This mechanical stimulation is transduced into electrical and chemical signals that are sent to the central nervous system. The CNS then responds by initiating changes that can include muscle relaxation, pain modulation, and alterations in local tissue dynamics.
What does the Evidence Suggest?
One study by Bove et al. (2019) investigates how the manipulation of fascial planes, which are integral to the biotensegrity structure of the body, can affect local and systemic inflammation and pain, highlighting the relationship between biomechanical input and biochemical and cellular responses (mechanotransduction).
Furthermore, research by Langevin et al. (2011) provides insight into how mechanical forces applied during manual therapy can lead to cellular changes that potentially affect back pain. The study suggests that the mechanical stretching of connective tissue during manual therapy could influence the local inflammation response and tissue repair, thus supporting the significance of mechanotransduction in manual therapeutic effects.
Additionally, a study by Chaudhry et al. (2008) uses mathematical modeling to demonstrate how mechanical forces are transmitted through the fascial system, supporting the concept of biotensegrity. This work helps to explain how localized treatment through manual therapy can have systemic effects due to the interconnectedness of the fascial network.
Integrating Theory with Practice
In practice, when a therapist applies a targeted technique such as myofascial release, they are engaging the biotensegrity system by manipulating the interconnected network of muscles and fascia. The force exerted is distributed through this network, affecting areas distant from the site of application. Mechanoreceptors within the fascia and muscles transduce this mechanical force into signals that the body interprets, leading to responses such as changes in muscle tension, pain relief, and alterations in cellular activities including gene expression and cytokine release.
In conclusion, biotensegrity provides a holistic view of the body’s structural organization, emphasizing the importance of whole-body interconnectedness, while mechanotransduction explains how mechanical forces are converted into biochemical signals, leading to a cellular response. The types of mechanoreceptors involved in manual therapy bridge these two concepts by responding to mechanical stimuli and initiating the transduction process, which ultimately results in the diverse therapeutic outcomes observed in manual therapy practices.
Manual Therapy, Perception, & The Nervous System
If you have not read Explain Pain by David Butler & Lorimer Mosley, then please do! It helps illustrate the relationship between the nervous system and perception. The relationship of perception and the nervous in the context of manual therapy is a fascinating and a complex area of study. Manual therapy techniques, such as massage, mobilization, or manipulation, are thought to influence the nervous system, which in turn affects an individual’s perception of pain, proprioception, and overall well-being.
Manual therapy exerts its effects through a variety of mechanisms, including mechanical stimulation of tissues, which in turn affects the nervous system. Sensory receptors within the skin, muscles, joints, and fascia—such as mechanoreceptors and nociceptors—are activated during manual manipulation. This activation triggers a cascade of neural responses that can modulate pain perception, alter proprioceptive feedback, and even influence autonomic functions.
One key aspect of how manual therapy affects perception is through the gate control theory of pain. This theory posits that non-painful input closes the “gates” to painful input, which prevents pain sensation from traveling to the central nervous system. Therefore, stimulation by manual therapy may “close the gates” by activating large-diameter nerve fibers that inhibit the transmission of pain signals carried by smaller-diameter fibers. A study by Melzack and Wall (1965) elucidates this concept and suggests that manual therapy may alleviate pain through this mechanism.
Further, manual therapy has been shown to induce changes in the autonomic nervous system. For instance, a study by Moraska and Chandler (2009) demonstrates that massage therapy significantly reduces heart rate, suggesting a shift towards a more relaxed state governed by the parasympathetic nervous system. This shift could be part of the reason patients often report a sense of relaxation and decreased stress following manual therapy.
Another dimension of the nervous system’s involvement is its role in proprioception, or the sense of the relative position of one’s own body parts. Manual therapy can enhance proprioception by stimulating mechanoreceptors in the joints and soft tissues. A study by Aimonetti et al. (2007) found that proprioceptive information processing from the hand is altered following manual therapy, indicating that the nervous system’s perception of body position and movement can be influenced by tactile manipulation.
Through the influence on the nervous system, manual therapy can alter the perception of pain, which is a complex sensory and emotional experience. When manual therapy stimulates the sensory receptors in tissues, it also engages the brain’s pain processing centers, potentially decreasing pain perception.
In summary, the relationship between the nervous system and perception in the context of manual therapy is mediated by various physiological mechanisms, including the modulation of sensory input, alteration of pain perception through the gate control theory, the impact on autonomic nervous system balance, and enhancement of proprioceptive feedback. These mechanisms collectively contribute to the therapeutic effects of manual therapy, affecting how pain and bodily sensations are perceived and processed by the nervous system.
Manual Therapy In Sports Rehab
Now that we have reviewed multiple perspectives on what is occurring when we provide manual therapy, the question becomes how do we apply manual therapy in sports rehab? Ultimately, in sports rehab I believe manual therapy is addressing (3) key principles
- Down-regulating peripheral tissue i.e. muscles, tendons, fascia
- Modulating perceptual symptoms and/or pain
- Teaching effective movement through tactile feedback
Down-Regulating Peripheral Tissue
The influence of the various biological process that we discussed above can lead to improved tissue tone by down-regulating specific tissues. If we apply the concepts of biotensegrity to appreciate it as a balancing act, then the joint limitations or limited range of motion can be viewed as an unbalanced equation between agonists and antagonists.
Whether you choose to provide joint mobilizations and stimulate joint receptors, utilize active release techniques to specific muscles, or spinal manipulations to stimulate the endocrine system – they’re all trying to provide an input to the body that provides balance around a joint.
Muscles that are “too tight” or “hypertonic” are tissues that probably need to be down-regulated in order to provide balance within the system. Concentric and eccentric orientation terminology is the same terminology has “short & tight” and “weak & long,” respectively. Choose your manual therapy method of choice, choose your language model, and ultimately restore balance in the system by modulating tension around a joint to improve range of motion or reduce pain.
Modulating Perceptual Symptoms or Pain
Pain and symptoms are both a subjective and emotional experience unique to each athlete or patient. Through the means of manual therapy we can modulate these symptoms or pain by tapping into some of the biological effects induced by manual techniques. Think of your parents putting their hand on your shoulder telling you “everything is going to be okay” right before you are about to try something challenging. Manual therapy can be just that for some athletes.
Their left hip flexor or TFL is tight producing hip impingement pain? Try a little active release to each of those muscles.
Their left ankle feel stiff and locked up? Try a quick anterior-posterior talocrural mobilization.
They are feeling a little unstable coming off of an ankle sprain? Use your hands to provide some compression around the ankle while the athlete goes through a split squat.
There are hundreds of techniques that we can use to help manage symptoms and pain. Each technique is tapping into one if not a few of the underlying biological processes that produce the desirable effect of reducing symptoms and pain.
Teaching Effective Movement
This final principle is my #1 intention for using manual therapy. Manual therapy techniques offer an opportunity to teach appropriate sensorimotor feedback to the athlete. Through the unique position of our hands and direction of force, we can educate athletes on what and how they should be feeling during certain exercises.
Trying to help an athlete avoid a pinching hip during a deadlift? Teach them what it feels like to appropriately shift into a hip while side lying.
An athlete keeps shifting away from an injured limb during a squat? Use your hands on their hips to provide specific tactile feedback to shift onto that affected side.
The possibilities are endless when it comes to movement correction and manual therapy. PNF – proprioceptive neuromuscular facilitation – is an incredibly under appreciated principle and is the foundation for all manual therapy targeting movement adaptations. Understand your hand placement, apply specific directional force, and the body will self-organize to achieve your desirable correction through manual therapy.
References
- Field, T., Hernandez-Reif, M., Diego, M., Schanberg, S., & Kuhn, C. (2005). Cortisol decreases and serotonin and dopamine increase following massage therapy. International Journal of Neuroscience, 115(10), 1397-1413.
- Rapaport, M. H., Schettler, P., Bresee, C. (2012). A preliminary study of the effects of repeated massage on hypothalamic-pituitary-adrenal and immune function in healthy individuals: a study of mechanisms of action and dosage. Journal of Alternative and Complementary Medicine, 18(8), 789-797.
- Uvnäs-Moberg, K., Handlin, L., Petersson, M. (2015). Self-soothing behaviors with particular reference to oxytocin release induced by non-noxious sensory stimulation. Frontiers in Psychology, 5, 1529.
- Bove, G. M., Chapelle, S. L., Hanlon, K. E., Diamond, M. P., & Mokler, D. J. (2019). Attenuation of inflammation and fibrosis by manual and instrument-assisted fascial manipulation in rat models of acute and chronic inflammation. Connective Tissue Research, 60(5), 1-13.
- Langevin, H. M., Fox, J. R., Koptiuch, C., Badger, G. J., Greenan-Naumann, A. C., Bouffard, N. A., … & Stevens-Tuttle, D. (2011). Reduced thoracolumbar fascia shear strain in human chronic low back pain. BMC Musculoskeletal Disorders, 12, 203.
- Chaudhry, H., Schleip, R., Ji, Z., Bukiet, B., Maney, M., & Findley, T. (2008). Three-dimensional mathematical model for deformation of human fasciae in manual therapy. Journal of the American Osteopathic Association, 108(8), 379-390.
- Melzack, R., & Wall, P. D. (1965). Pain mechanisms: a new theory. Science, 150(3699), 971-979.
- Moraska, A., & Chandler, C. (2009). Changes in clinical parameters in patients with tension-type headache following massage therapy: a pilot study. Journal of Manual & Manipulative Therapy, 17(2), E80-E89.
- Aimonetti, J. M., Hospod, V., Roll, J. P., & Ribot-Ciscar, E. (2007). Cutaneous afferents provide a neuronal population vector that encodes the orientation of human ankle movements. Journal of Physiology, 580(Pt 2), 649-658.



