Approximate Read Time: 19 minutes
“BFR training tricks the body into thinking it’s lifting heavy—delivering strength and hypertrophy gains at light loads, when injured joints and tissues can’t tolerate stress.”
What You will learn
- Why BFR accelerates strength and limits atrophy after surgery
- Safe application methods for post-op and acute rehab phases
- Research-backed outcomes for muscle, tendon, and joint recovery
What Is Blood Flow Restriction Training?
Imagine a way to gain the benefits of heavy squats or leg presses without ever loading more than 20–30% of your one-rep max. That’s the promise of blood flow restriction (BFR) training. By using a pneumatic cuff or elastic band at the upper arm or thigh, blood flow into a limb is reduced and venous return is partially occluded. The result is a hypoxic, metabolically stressful environment where muscles behave as if they’re lifting heavy—even though the load is light (Mattocks et al., 2018).
“BFR gives post-op patients the benefits of heavy lifting—without the heavy loads.”
This technique, first popularized in Japan as “KAATSU training,” has moved far beyond the gym (Loenneke et al., 2012). In the rehab setting, it is now a critical tool for post-operative patients and athletes recovering from acute injuries who cannot tolerate heavy loads (Loenneke et al., 2018).
The Science of BFR: Mechanical Tension vs. Metabolic Stress
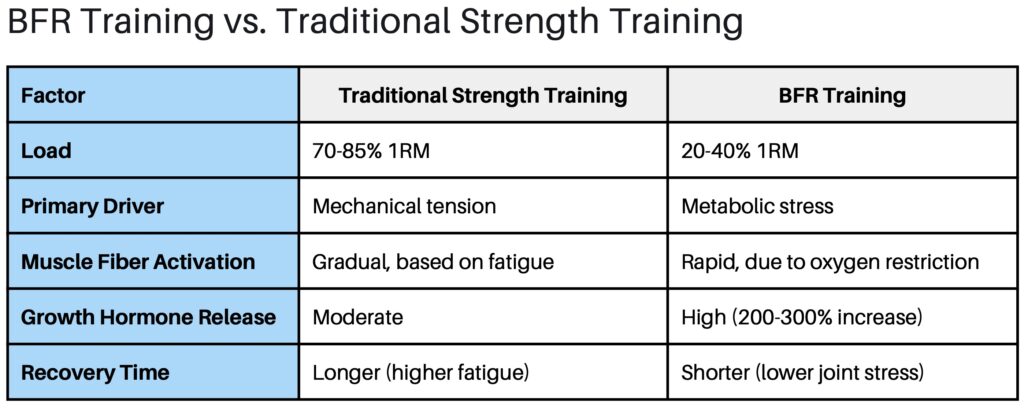
Muscle adaptation has two main pathways: mechanical tension and metabolic stress (Loenneke et al., 2012). Traditional strength training leans on mechanical tension—placing high loads on muscle fibers that trigger hypertrophy and protein synthesis. But for a patient who just had ACL surgery or is recovering from a tendon repair, those heavy loads aren’t safe.
BFR instead leverages the metabolic stress pathway. By restricting venous return, metabolites like lactate and hydrogen ions accumulate. This environment drives a surge in growth hormone (GH) and insulin-like growth factor-1 (IGF-1), both powerful anabolic signals (Mattocks et al., 2018). The muscle “feels” like it’s working under extreme load, recruiting fast-twitch fibers earlier than usual despite the light weight (Loenneke et al., 2012).
Meta-analyses confirm the effect: low-load BFR training (20–40% 1RM) can stimulate hypertrophy and strength gains comparable to traditional high-load lifting (70–85% 1RM) (Loenneke et al., 2012). This is a game-changer in early rehab phases, when preventing muscle atrophy is the priority.
“By amplifying metabolic stress, BFR convinces the body it’s lifting heavy—even when it’s not.”
A clear example comes from patients recovering after anterior cruciate ligament (ACL) reconstruction. Quadriceps atrophy is common and can persist for months post-surgery. BFR applied during simple knee extensions or straight leg raises helps maintain muscle size and function at a time when heavy loading isn’t possible (Ohta et al., 2003; Tennent et al., 2017).

BFR in Post-Operative Rehab: Fighting Muscle Atrophy
One of the greatest challenges following surgery is the rapid decline in muscle size and strength due to immobilization or reduced loading. Research shows that muscle cross-sectional area can decrease within the first two weeks of disuse (Takarada et al., 2000). This loss is particularly evident after procedures like ACL reconstruction, meniscus repair, or cartilage restoration.
BFR has emerged as one of the most effective tools to counteract this atrophy. Studies demonstrate that combining low-load resistance exercise with BFR (20–30% 1RM) produces similar hypertrophy and strength outcomes to high-load training (70–85% 1RM), which would otherwise be contraindicated in the early phases of rehab (Loenneke et al., 2012).
For example, Ohta et al. (2003) reported that patients recovering from ACL reconstruction who performed low-load knee extensions with BFR experienced significantly greater quadriceps strength and muscle mass than those who performed the same exercises without BFR. These findings are consistent across multiple randomized controlled trials showing improved outcomes in post-op patients with BFR integration (Tennent et al., 2017).
Acute Injury Applications: Healing Without Heavy Loads
Beyond the surgical setting, BFR is also useful in the acute injury phase, when high mechanical loads could aggravate tissues. Conditions like patellofemoral pain, acute muscle strains, or ankle sprains often present this dilemma: patients need strength, but heavy loading is painful or unsafe.
Low-intensity BFR can bridge this gap. Giles et al. (2017) showed that patients with patellofemoral pain who performed quadriceps strengthening under BFR not only improved muscle function but also reported reduced pain compared to those performing high-load training. Similarly, early use of BFR after hamstring strain or calf injury may allow for meaningful strength preservation without provoking further tissue damage (Hughes et al., 2017).
By targeting metabolic stress without mechanical overload, BFR provides a novel way to stimulate adaptation during phases when standard strengthening protocols would be too aggressive.

Safety, Cuffs, and Pressures: Getting BFR Right
With all its benefits, clinicians often raise a fair question: is BFR safe? Controlled research has consistently found that when performed with appropriate equipment and pressures, the risks are minimal (Loenneke et al., 2011; Mattocks et al., 2018).
“The safest BFR isn’t about high pressure—it’s about the right pressure for the right cuff and the right person.”
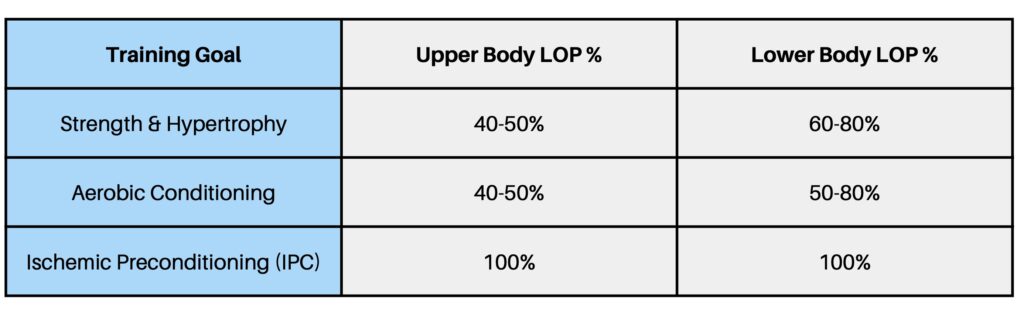
The key lies in cuff selection and individualized pressure. Wide cuffs require less pressure than narrow cuffs to achieve the same level of occlusion (Jessee et al., 2016). Limb Occlusion Pressure (LOP)—the minimum pressure needed to stop arterial inflow—should be measured for each athlete, and BFR should be applied at a percentage of LOP (typically 40–50% for upper body, 60–80% for lower body).
Using arbitrary pressures (e.g., inflating all cuffs to 200 mmHg) is outdated and can elevate cardiovascular stress unnecessarily (Rossow et al., 2012). When individualized pressures are used, the cardiovascular and perceptual responses are well within safe ranges (Jessee et al., 2017).
Aerobic and Recovery Applications of BFR
BFR isn’t limited to resistance exercise. Aerobic training under partial occlusion has shown surprising benefits, especially for patients who cannot tolerate running or high-impact activity.

For example, low-intensity cycling at ~40% VO₂max with BFR has been shown to increase thigh muscle size and aerobic capacity (Abe et al., 2010). Similarly, BFR walking protocols (20 minutes at moderate pace) improved quadriceps cross-sectional area and aerobic performance in older adults (Ozaki et al., 2011). These adaptations are remarkable because such low intensities, performed without BFR, would normally be insufficient to drive muscle hypertrophy.
The other fascinating frontier is ischemic preconditioning (IPC)—short bouts of BFR applied without exercise. IPC can enhance mitochondrial efficiency, improve blood flow, and prime muscles for subsequent performance (Loenneke et al., 2012). Clinically, IPC has been used to accelerate recovery post-exercise and may even support healing after surgery by reducing oxidative stress and inflammation (Mouser et al., 2020).
BFR turns a walk in the park—or even sitting with cuffs—into a stimulus for growth and recovery.”
Evidence From Clinical Research
BFR has been studied extensively over the last decade, and systematic reviews consistently support its clinical use.
- Strength & Hypertrophy: A landmark meta-analysis found that low-load BFR training (20–40% 1RM) produces significant increases in muscle strength (effect size 0.58) and hypertrophy (effect size 0.39), while traditional low-load training without BFR produced no meaningful changes (Loenneke et al., 2012).
- Post-Operative Rehab: A systematic review of musculoskeletal rehab concluded that BFR is an effective adjunct to mitigate atrophy and promote early strength gains after surgeries like ACL reconstruction, arthroscopy, or tendon repair (Hughes et al., 2017).
- Safety: A critical review showed no greater risk of clotting, rhabdomyolysis, or cardiovascular harm than traditional resistance training, when performed with appropriate cuff widths and individualized pressures (Loenneke et al., 2011).
Collectively, this body of evidence positions BFR as an effective strategy for rehabilitation when heavy loading is unsafe or contraindicated.
Nutrition + BFR: Optimizing the Healing Environment
Rehabilitation is not just about exercise stimulus—it’s about creating the right internal environment for tissue repair. That’s where nutrition and BFR complement one another.
BFR amplifies the metabolic stress pathway, creating surges in growth hormone and IGF-1 (Mattocks et al., 2018). To take advantage of this, we need adequate protein and micronutrient support to build new muscle proteins. As Danielle LaFata emphasized on Finding Small Wins, protein distribution across the day (0.8–1.0 g per lb of body weight) paired with antioxidant-rich foods helps preserve lean mass while managing inflammation.
This synergy means the rehab team must think beyond exercise prescription. Combining evidence-based nutrition with mechanical stressors like BFR ensures both the “materials” and the “builders” for tissue repair are in place.
For a deeper dive into fueling recovery, check out Muscle Strain and Nutrition: A Complete Guide to Maximize Recovery.
Practical Guidelines for Therapists, Trainers, and Certified Coaches
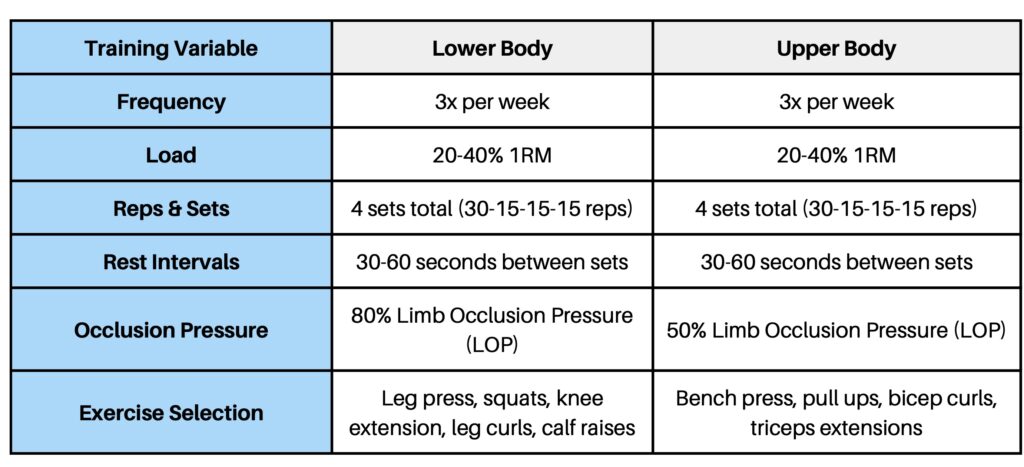
The best BFR programs are precise: the right cuff, the right pressure, and the right exercise at the right time. Here are evidence-based guardrails to safely and effectively start using BFR training today:
- Cuff Selection: Wide pneumatic cuffs (≥10 cm) are preferred for consistency; elastic bands can be used but are harder to standardize (Jessee et al., 2016).
- Pressure Prescription: Base occlusion pressure on Limb Occlusion Pressure (LOP), not arbitrary numbers. Aim for 40–50% LOP upper body, 60–80% LOP lower body (Loenneke et al., 2012).
- Exercise Prescription: Resistance loads at 20–40% 1RM, following the “30-15-15-15” scheme (75 reps total) are widely validated (Mattocks et al., 2018).
- Frequency: 2–3x per week appears optimal, balancing adaptation and recovery (Loenneke et al., 2012).
- Integration: Combine BFR with manual therapy, neuromuscular stimulation, or aerobic work to layer adaptations without overloading tissue (Mouser et al., 2020).
Conclusion
Blood flow restriction training has shifted from a niche concept to a cornerstone of modern rehabilitation. For post-operative patients and athletes navigating the acute injury phase, it provides a safe and effective bridge—delivering the benefits of heavy lifting at light loads. Here are the key lessons to carry forward:
- BFR mimics heavy lifting by amplifying metabolic stress at light loads.
- It prevents atrophy post-op, keeping the hypertrophy switch “on” when mechanical loading isn’t possible.
- It reduces pain and preserves function in acute injuries like patellofemoral pain or early tendon loading.
- Safety lies in precision—cuff width, individualized limb occlusion pressure, and evidence-based protocols matter.
- BFR is versatile—from resistance training to aerobic work and recovery, it expands the rehab toolbox.
Think of BFR as a way of tricking the body. You’re not loading 300 lbs on a barbell, but metabolically, the muscle is convinced you are. For an ACL patient struggling to regain quad strength, or an athlete sidelined by tendon pain, this can mean the difference between decline and progress.
Free Download
Watch More Like This
Read More Like This
Related Podcasts
References
Mattocks KT, Jessee MB, Mouser JG, et al. The application of blood flow restriction: lessons from the laboratory. Curr Sports Med Rep. 2018;17(4):129-134. doi:10.1249/JSR.0000000000000475
Loenneke JP, Wilson JM, Marin PJ, Zourdos MC, Bemben MG. Low intensity blood flow restriction training: a meta-analysis. Eur J Appl Physiol. 2012;112(5):1849-1859. doi:10.1007/s00421-011-2167-x
Hughes L, Paton B, Rosenblatt B, Gissane C, Patterson SD. Blood flow restriction training in clinical musculoskeletal rehabilitation: a systematic review and meta-analysis. Br J Sports Med. 2017;51(13):1003-1011. doi:10.1136/bjsports-2016-097071
Mouser JG, Loenneke JP, Valenzuela PL, Jiménez-Pavón D, Bemben MG. Blood flow restriction training and muscle health in aging: a review of current research. Aging Dis. 2020;11(4):787-804. doi:10.14336/AD.2019.0817
Ohta H, Kurosawa H, Ikeda H, et al. Low-load resistance muscular training with moderate restriction of blood flow after anterior cruciate ligament reconstruction. Acta Orthop Scand. 2003;74(1):62-68. doi:10.1080/00016470310013680
Tennent DJ, Hylden CM, Johnson AE, Burns TC, Wilken JM, Owens JG. Blood flow restriction training after knee arthroscopy: a randomized controlled pilot study. Clin J Sport Med. 2017;27(3):245-252. doi:10.1097/JSM.0000000000000377
Giles L, Webster KE, McClelland J, Cook J. Quadriceps strengthening with and without blood flow restriction in the treatment of patellofemoral pain: a double-blind randomized trial. Br J Sports Med. 2017;51(23):1688-1694. doi:10.1136/bjsports-2016-096329
Jessee MB, Buckner SL, Mouser JG, et al. The influence of cuff width, sex, and race on arterial occlusion: implications for blood flow restriction research. Sports Med. 2016;46(6):913-921. doi:10.1007/s40279-016-0477-6
Rossow LM, Fahs CA, Sherk VD, et al. The effect of acute blood-flow-restricted resistance exercise on postexercise blood pressure. Clin Physiol Funct Imaging. 2011;31(6):429-434. doi:10.1111/j.1475-097X.2011.01031.x





