Approximate Read Time: 20 minutes
“Every movement is a conversation between sensation and action—PNF teaches us to listen more clearly.”
What You will learn
- PNF uses sensory feedback to optimize strength and coordination.
- Diagonal and spiral patterns mimic natural human movement.
- Orthotics and manual therapy amplify PNF’s role in performance.
What Is Proprioceptive Neuromuscular Feedback?
Proprioceptive Neuromuscular Feedback (PNF) is more than a stretch routine—it’s a language system between your body and your brain. At its core, PNF is about improving how the nervous system interprets sensory input to generate precise, coordinated motor output. For rehab and performance professionals, it represents a bridge: where neurophysiology meets practical movement.
PNF asks a simple but profound question: if movement is communication, how can we sharpen the signal?
The Origins of PNF: A Neurological Beginning
PNF began in the 1940s with Dr. Herman Kabat, who wasn’t trying to create a sports performance tool but a clinical therapy for neurological disorders such as polio. Kabat recognized that the body’s reflexes could be harnessed to restore coordination. His work showed that by manipulating proprioceptive feedback—the sensory system that tells us where our body is in space—therapists could spark better motor patterns.
What started as a lifeline for neurological patients soon migrated into sports medicine and strength training. Today, athletic trainers, physical therapists, and performance coaches use PNF as a method to improve flexibility, strength, and motor control (Lephart et al., 1997).
“PNF didn’t start on the field—it began in neurology labs, proving rehab and sport are closer cousins than we think.”
The Proprioceptive System: The Body’s GPS
To understand PNF, you first have to respect proprioception. Think of proprioception as the body’s internal GPS. It’s made possible by specialized sensors—muscle spindles that detect stretch, and Golgi tendon organs that detect tension. Together, they send constant updates to the brain about limb position, muscle length, and joint angle (Lam & Pearson, 2002).
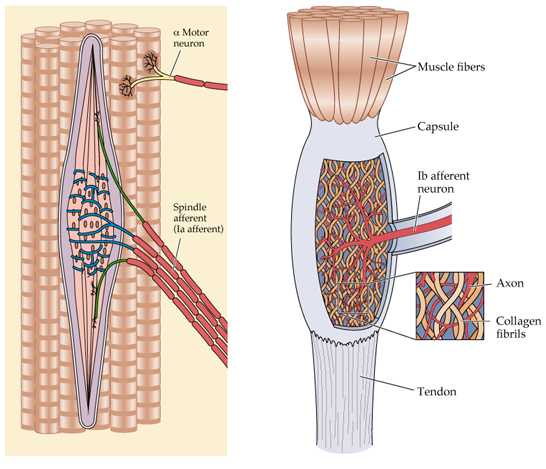
When these receptors are engaged through resistance, stretching, or pressure, the nervous system adapts. That adaptation is what we harness in rehab. PNF techniques deliberately stimulate these sensors to create new motor responses.
This is where reciprocal inhibition comes in. Contracting one muscle group silences its opposite, allowing for smoother, freer motion. A hamstring contracts? The quadriceps relax, giving you more range of motion. It’s like the body’s version of noise-cancelling headphones, silencing interference so movement can flow.
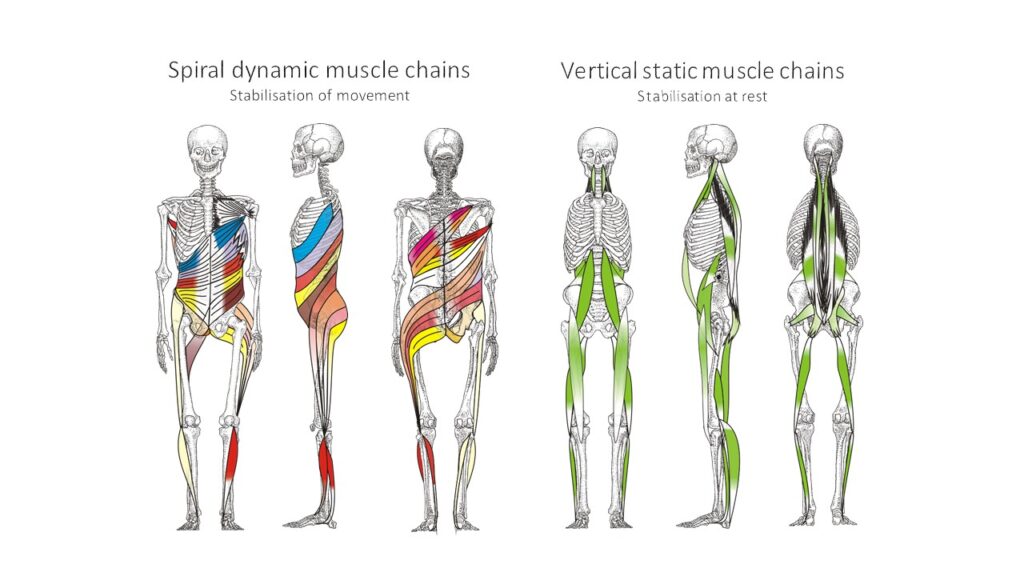
Spirals, Diagonals, and Why Straight Lines Fail Us
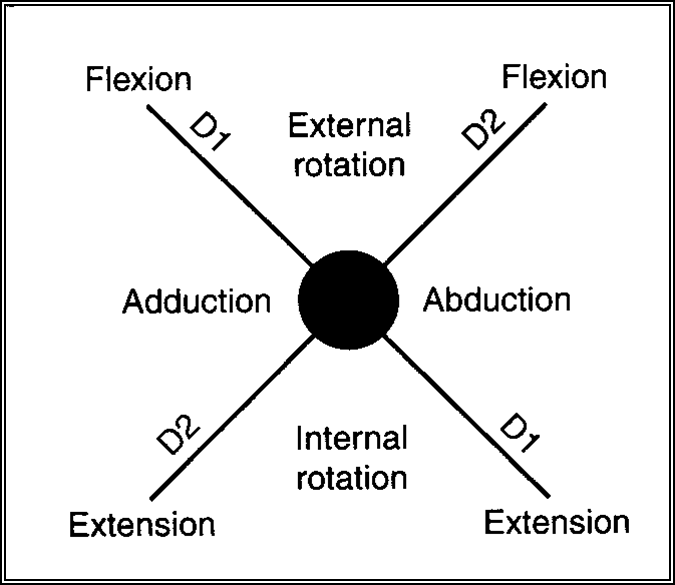
Life doesn’t happen in straight lines. Walking, reaching, throwing, sprinting—all of these require diagonal, spiral-like movements. Kabat and his contemporaries designed PNF patterns around these natural shapes, tapping into the body’s preference for tri-planar motion (Lephart, Pincivero, & Rozzi, 1998).
“Spiral patterns in PNF are less about artful geometry and more about biological truth.”
Linear training—think traditional bicep curls—can strengthen tissue, but it doesn’t always transfer to functional movement. PNF patterns, by contrast, mimic the choreography of sport and life. When an athlete plants to change direction, they’re not just flexing and extending. They’re spiraling through hips, torso, and shoulders in a coordinated symphony.
The Physiology Behind PNF: More Than Stretching
It’s easy to mistake PNF for fancy stretching. But under the hood, the physiology is rich. At its foundation are three contraction types—isometric, concentric, and eccentric—each influencing proprioceptive feedback differently.
- Isometric contractions (muscle length doesn’t change) help stabilize a joint and send prolonged proprioceptive signals, reinforcing position awareness.
- Concentric contractions (muscle shortens) enhance strength and coordination by recruiting motor units through force production.
- Eccentric contractions (muscle lengthens under load) create some of the strongest proprioceptive responses, teaching the nervous system how to control deceleration.
When combined in PNF patterns, these contractions stimulate synaptic plasticity—the nervous system’s ability to rewire itself through repeated input (Mulder & Hulstijn, 1985). That plasticity is what allows a newly restored ankle to “remember” how to stabilize on uneven turf or a post-op ACL to trust eccentric control when decelerating.
“PNF is not a stretch—it’s a neurological rehearsal.”
In short, PNF works because it nudges the nervous system to rehearse more efficient scripts until those scripts become automatic.
Orthotics and Apparatus: Tools That Talk to the Nervous System
Performance therapists often default to thinking of external devices—orthotics, kettlebells, barbells—as mechanical tools. But in reality, they are neurological influencers.
Take a mouthguard. To most, it’s just a piece of plastic. But shifting jaw alignment alters sensory input at the temporomandibular joint, changing posture and even muscle recruitment patterns downstream. Similarly, shoe inserts can adjust pressure distribution at the foot, which subtly alters center of mass, gait mechanics, and joint loading (Lephart et al., 1997).

Weights tell a similar story. A kettlebell swing isn’t just about posterior chain strength. The offset load forces the body to stabilize rotational forces, flooding proprioceptors with sensory data. Barbells challenge the system differently, demanding symmetrical control across a linear axis. Both are “speaking” to proprioception, shaping motor output.
Think of these tools as conversation starters for the nervous system: they create sensory “noise” that forces the body to adapt and coordinate. That’s PNF in action—just dressed up as strength training.
Manual Therapy and PNF: Two Sides of the Same Coin
Manual therapy and correctives often get siloed in professional circles. One belongs in the “hands-on” camp, the other in the “exercise” camp. But when viewed through the lens of proprioception and PNF, they are simply two variations on the same theme.
“Manual therapy primes the canvas; PNF paints the movement.”
A skilled therapist applying deep tissue mobilization is stimulating mechanoreceptors, much like a PNF diagonal pattern stimulates muscle spindles. Both are sensory interventions designed to provoke motor responses.
For example, pressing into the quadriceps with sustained pressure can trigger Golgi tendon organ-mediated relaxation. Add a PNF spiral pattern immediately after, and you’re reinforcing that relaxation with coordinated motor learning (Mulder & Hulstijn, 1985).
This marriage—manual therapy plus PNF—isn’t about redundancy. It’s about coherence. One primes the sensory system, the other programs it. When layered, they create a more durable movement solution.
Sensorimotor Modulation: Optimizing Posture and Movement
One of PNF’s superpowers is its role in sensorimotor modulation—tuning the body’s responses to achieve desired joint positions and postures. In other words, it teaches the body how to “manage pressure.”
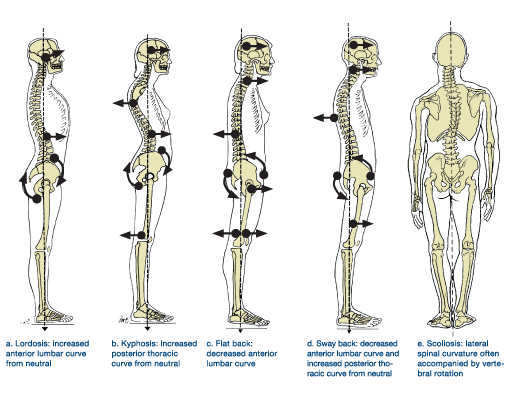
Imagine standing on a wedge during a squat. That subtle change in angle shifts your center of mass, creating a new stream of proprioceptive input. The nervous system recalibrates, and suddenly a stubborn hip impingement eases or a faulty trunk lean resolves.

These adjustments, whether through ramps, wedges, or orthotics, aren’t gimmicks. They are methods of modulating sensory feedback so the motor system learns a cleaner pattern. When used systematically, they allow therapists to guide athletes back to function with precision.
For a deeper dive into posture and pressure management, check out Does Perfect Posture Exist?
Functional Spirals in Sport and Life
It’s worth zooming out here. Why obsess over spirals and diagonals? Because they’re everywhere. A pitcher’s throw, a sprinter’s acceleration, even reaching into the back seat of your car—all rely on rotational spirals.
Kabat didn’t invent this idea; biology did. PNF simply translated it into a systematic practice. That’s why PNF feels so intuitive in sports rehab—it mimics the language the body already speaks.
When a rehab exercise looks like life, transfer improves. A resisted PNF diagonal is not just a rehab drill; it’s rehearsal for the messy, multi-planar chaos of sport.
Practical Applications of PNF in Rehab
The beauty of PNF is that it scales across the rehab continuum—from early-stage recovery to high-performance return-to-play.
- Early Rehab: In the acute or subacute phase, PNF can restore basic neuromuscular coordination. Gentle diagonal patterns, paired with isometrics, help re-establish joint awareness after swelling or immobilization (Lephart, Pincivero, & Rozzi, 1998).
- Intermediate Stages: As tissue tolerance improves, eccentric contractions within PNF spirals prepare the body for load absorption—critical for athletes approaching running or deceleration progressions.
- Return to Play: Late-stage rehab leverages PNF patterns under high load and speed. Think resisted diagonal lifts, spiral lunges, or medicine ball throws that mimic the specific mechanics of sport.
The through-line is that PNF doesn’t just restore motion—it restores movement confidence. Athletes often say after PNF-driven rehab sessions: “I trust my knee again.” That trust is the nervous system recalibrating.

PNF in Performance Training: Not Just for Injury
Too often, PNF gets pigeonholed as a rehab tool. But its principles apply equally in strength and conditioning.
A split squat with a kettlebell held contralateral to the front leg isn’t “just” strength—it’s a PNF-inspired pattern, forcing diagonal stability through the trunk and hip. Similarly, rotational medicine ball throws replicate the spiral actions of sprinting or pitching.
“Performance training isn’t separate from PNF—it’s PNF at higher speeds and loads.”
Even traditional lifts, when viewed through the lens of proprioception, are PNF variations. Every barbell squat, every push press, every lunge challenges proprioceptors to integrate sensory input into controlled motor output.
In other words: the weight room is already filled with PNF. The distinction lies in whether a coach recognizes and harnesses it.
The Role of Orthotics and Equipment in Long-Term Success
Orthotic devices often get dismissed as band-aids. But in the 3P Framework, they’re amplifiers of sensory input.

A wedge under the heel? That’s not “cheating” the squat—it’s reshaping proprioceptive input to improve coordination. A mouthguard? It’s not just tooth protection—it’s a proprioceptive cue for posture. Shoe inserts? They’re tools to redistribute pressure and guide gait mechanics (Lam & Pearson, 2002).
What matters is coherence. When orthotics, manual therapy, and exercise are all pulling on the same PNF principles, outcomes improve. The system becomes less about isolated interventions and more about an integrated sensory-motor approach.
PNF as a Philosophy, Not Just a Technique
Perhaps the most important takeaway: PNF is not a single exercise or stretch. It’s a philosophy of movement. It says:
- Every movement is shaped by sensory input.
- Every joint position can be optimized through proprioception.
- Every athlete or patient can “learn” better motor scripts with the right feedback.
This philosophy forces us to view rehab not as restoring tissue in isolation, but as retraining the body’s conversation between sensation and action.
PNF isn’t a fringe rehab tool or a dated stretching technique. It’s a powerful framework rooted in the body’s sensory systems and motor learning pathways.
Let’s revisit the big lessons:
- PNF leverages proprioception—our body’s GPS—for better motor control (Mulder & Hulstijn, 1985).
- Diagonal and spiral patterns mirror real-world sport and life, creating natural transfer.
- Manual therapy + PNF is about coherence—priming and programming together.
- Orthotics and apparatus aren’t accessories; they’re proprioceptive amplifiers.
- PNF is philosophy, a way of viewing movement as sensory-driven communication.
If we embrace PNF as a lens—rather than a checklist of drills—we unlock a more integrated, adaptive way to treat injuries and build performance.
WANT TO LEARN MORE ABOUT PNF?
Check out my Performance Therapy Mentorship for case studies and techniques that show you how to integrate PNF into your rehab and training.
Read More Like This
Related Podcasts
References
Mulder T, Hulstijn W. Sensory feedback in the learning of a novel motor task. J Mot Behav. 1985;17(1):110-28. doi:10.1080/00222895.1985.10735340
Lam T, Pearson K. The role of proprioceptive feedback in the regulation and adaptation of locomotor activity. Adv Exp Med Biol. 2002;508:343-55. doi:10.1007/978-1-4615-0713-0_40
Lephart S, Pincivero D, Giraido J, Fu F. The Role of Proprioception in the Management and Rehabilitation of Athletic Injuries. Am J Sports Med. 1997;25:130-137. doi:10.1177/036354659702500126
Lephart S, Pincivero D, Rozzi S. Proprioception of the Ankle and Knee. Sports Med. 1998;25:149-155. doi:10.2165/00007256-199825030-00002





