Approximate Read Time: 10 minutes + Free Download
“In modern chondromalacia rehab, numbers tell part of the story — but integrating them with history, biology, and the right interventions unlocks the path forward.”
What You will learn
- Integrating objective data with history optimizes rehab.
- Isokinetic and isometric testing offer unique value.
- Managing recurrent swelling is central to longevity.
- Orthobiologics can fill the treatment gap.
- Gradual exposure prevents setbacks in return to play.
Understanding the Player’s Baseline: History Shapes the Plan
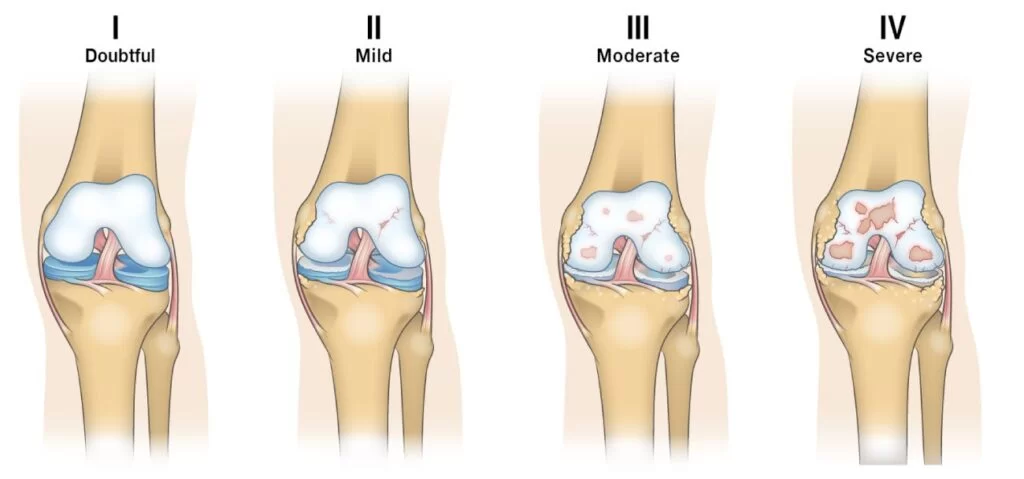
By the time this NBA basketball player walked into the gym for testing, the numbers were only part of what I needed to know. His right knee had been through multiple surgeries. The MRI confirmed what we already suspected from years of playing and clinical observation — a grade III chondromalacia. On top of that, there was the recurring swelling that would surface after intense workloads when we would try to progress the plan.
We’d spent the first eight weeks post-operatively of a recent surgery on fundamentals: calming the joint, reestablishing quadriceps tone, and restoring basic movement patterns. The goal was simple — no cutting drills, no scrimmaging, until swelling was under control and the knee moved fluidly under bodyweight. Once those pieces were in place, it was time to see exactly what the joint could do under load. This staged return followed the framework outlined in the 3P Model: Sports Rehab Framework for Results.
How Isometric and Isokinetic Testing Can Guide Decision Making
Two of the more commons reasons why a post-surgical knee will continue to swell during rehab are:
- Poor quadriceps strength: muscles act as the tension cables and shock absorbers for joints. The quadriceps are the main shock absorber in the knee. If the quadriceps is weak, then the joint will take the bulk of the stress from impact that can lead to recurrent swelling.
- Low stress tolerance: just like soreness you get from “getting back into it” with your workouts after a vacation, joints undergo the same unloading and reloading cycle. Do too much in your first workout after a vacation, you are very sore for days. Do too much during rehab, the knee joint can swell. Joints, just like muscles and tendons, need gradual exposure to stress too. If the stress is too much, then swelling usually increases from poor tolerance to stress.
I needed to understand if this recurrent swelling after intense court workouts was a local muscle problem or global loading problem. This is where isokientic and isometric testing came into play.
The athlete sat in the HUMAC Norm, and we started with an isometric knee extension test at 90 degrees. The output was strong: 284 ft-lb on the right (114% bodyweight) and 274 ft-lb on the left (110% bodyweight), leaving only a 4% deficit. Average torque was symmetrical and was hitting the minimum standard of 100% bodyweight.
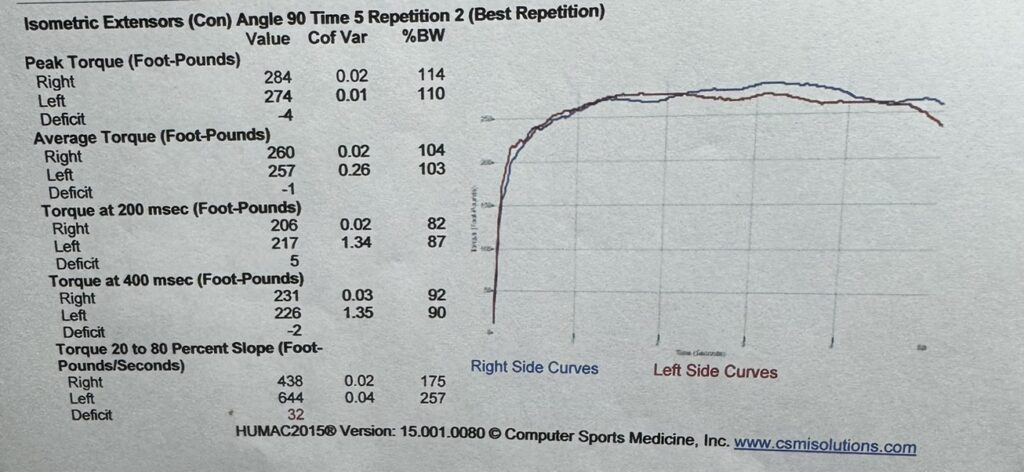
The isokinetic testing at 60°/sec painted a complementary picture. Extensor torque was virtually identical — 203 ft-lb on the right, 205 on the left — and both landed just over 80% of body weight. Not a perfect score as the standard I would like to see is 100% bodyweight. I have seen very tall athletes struggle to obtain the 100% bodyweight standard because of the larger moment arm from having larger legs.
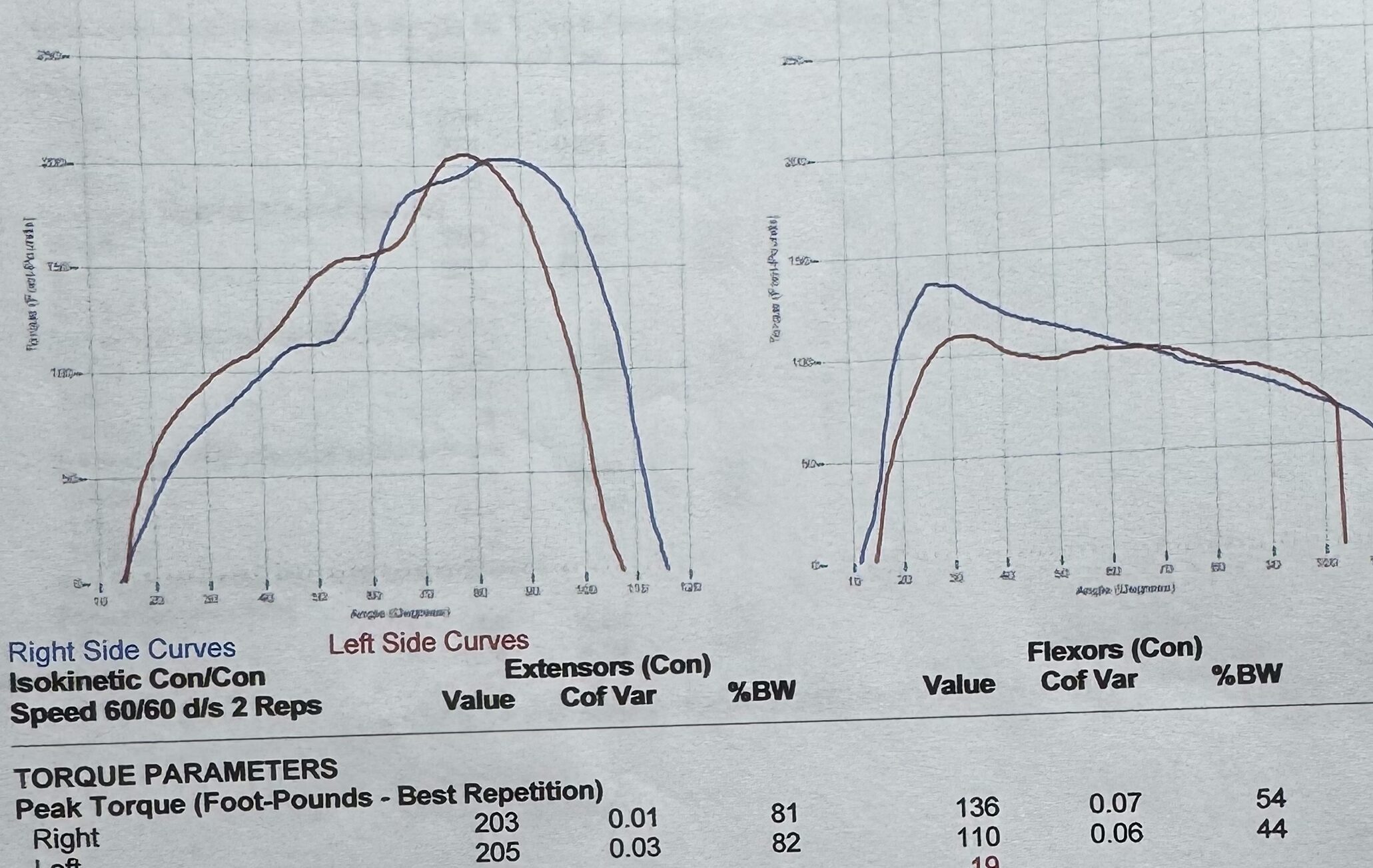
Back to the original question of is this a local muscle problem or a global loading problem? These scores are good enough to indicate that the local tissue qualities are where they are and that this is more of a global loading problem.
WANT TO LEARN MORE ABOUT ISOKINETIC TESTING: These testing approaches and interpretations are covered in depth in the Ultimate Guide to Isokinetic Testing: Enhancing Sports Rehabilitation and Performance and further explored in my conversation with Daniel Bodkin on the Isokinetic Testing and Assessment in Sports episode of Finding Small Wins.
The Keystone Variable: Managing Swelling in a High-Load Joint
If you’ve worked with elite knees, you know the cycle: load increases, swelling follows, quadriceps tone drops, force absorption falls off, and joint stress rises. We were determined not to get caught in that loop.
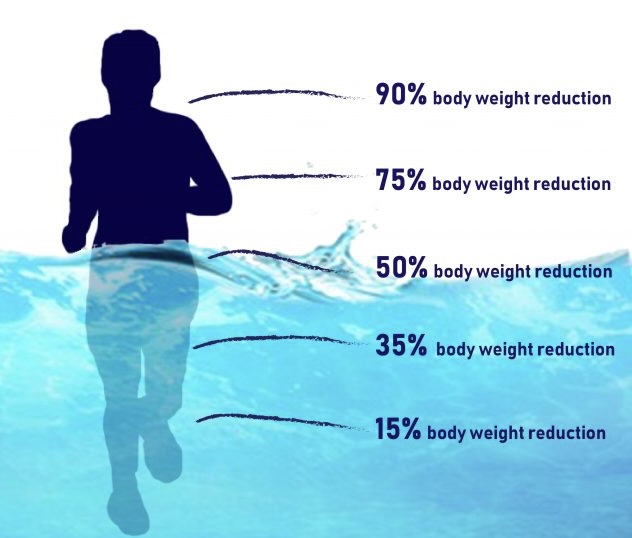
Our plan was proactive. The athlete wore a compression sleeve daily and used a GameReady unit for targeted compression after practices. We built in recovery sessions that featured pool exercise and cycling to maintain cardiovascular output without pounding the joint.

Neuromuscular stimulation sessions helped keep quad fibers firing even on lower-load days. Every intervention was aimed at breaking the cause-and-effect chain between load and swelling — a principle I outlined in How to Accelerate Injury Recovery by Effectively Managing Swelling.
Why We Chose Hyaluronic Acid for This Knee
When it came to biologic interventions, we had options. Platelet Rich Plasma (PRP) and Alpha-2 Macroglobulin (A2M) were on the table to help reduce inflammation, slow down cartilage degeneration, and improve healing. Bone Marrow Aspirate Concentrate (BMAC) was another possibility but more invasive and costly. But each tool has a time and a place, and in this moment, hyaluronic acid (HA) made the most sense.
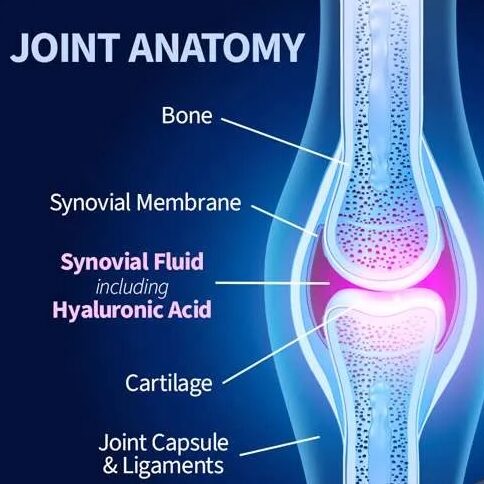
The joint’s cartilage surface was already compromised, and the chondromalacia meant that lubrication and shock absorption inside the joint space were at a premium. Hyaluronic acid, a naturally occurring lubricant in synovial fluid, could help restore viscosity, improve joint mechanics, and modulate inflammation without provoking the kind of post-injection flare you sometimes see with PRP.
The literature backed it up. The 2018 Altman review showed that repeated HA courses can reduce pain and maintain improvements without increasing adverse events, even over extended treatment cycles. During a progressive rehab program where the biggest threat to this player’s availability was swelling after load, HA offered a direct way to improve the joint environment without adding unnecessary recovery days. This strategy aligns with insights from the Stem Cells, Exosomes, Peptides, and Orthobiologics ft. Dr. Chuck Peterson and Dr. Cameron Davis episode of Finding Small Wins.
Orthobiologics in the Middle Ground
In the Dr. Peterson and Dr. Davis conversation, they describe orthobiologics as the “middle ground” — the space between NSAIDs or cortisone on one end, and surgery on the other. For degenerative cartilage changes, HA and A2M can preserve and support tissue quality. For tendinopathies, PRP or BMAC may be the better fit.
For this player, cortisone would have been a short-term fix with potential long-term costs to cartilage integrity. PRP could have been valuable later, but the immediate problem wasn’t healing — it was joint homeostasis. HA’s role here was strategic. For more on how to match the right intervention to the right limitation, see 4 Pillars of Sports Rehab.
From Data to a Plan: Why We Moved to On-Court Work
When we put the test results next to the clinical picture, the logic was clear. The athlete had symmetrical quadriceps strength, peak torque at or above 110% body weight isometrically, and a favorable hamstring-to-quad ratio. The only yellow flag was the slower rate of force development on the right side — something we could address progressively as we reintroduced game-like stimuli.
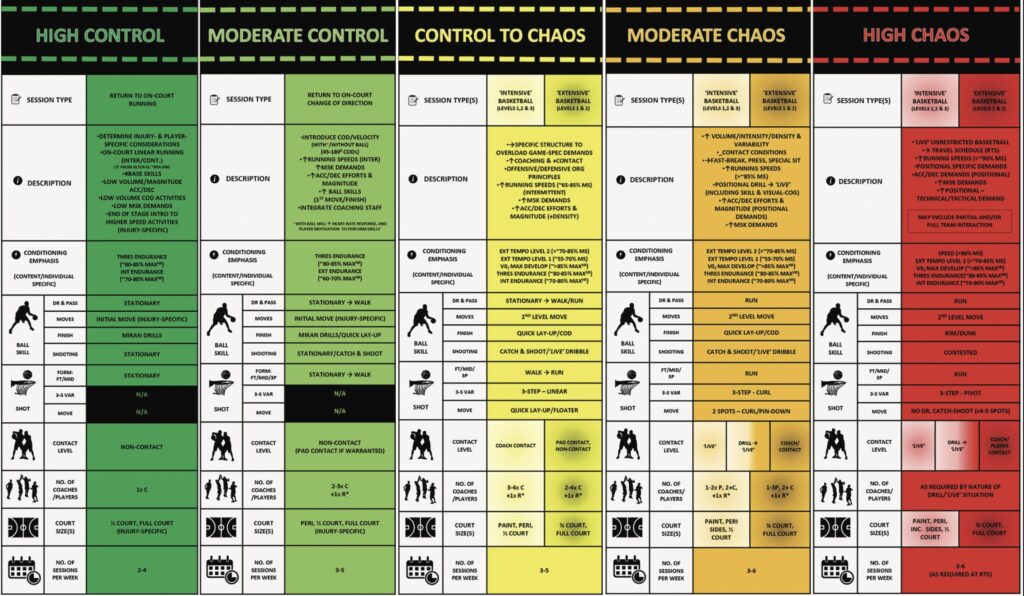
We mapped out a six-week on-court progression rooted in the 3P Framework and the Control-Chaos Continuum. The first phase was all non-contact, small-space drills where pace and workload could be tightly controlled. From there, we expanded to small-sided games, increasing both the space and the unpredictability. Full-court live play came last, with minutes carefully limited and swelling monitored after each session.
This wasn’t just about getting back to the game; it was about building a runway long enough to sustain performance without constant setbacks. A similar principle is outlined in How the Triple Hop Misses Eccentric Strength & Deceleration Prep, which explains why return-to-play readiness is more than passing a hop test.
Lessons for the Broader Field
This case reinforced something I’ve seen repeatedly: testing is a compass, not a map. Isometric and isokinetic tools tell you where you are, but they have to be interpreted through the lens of an athlete’s history, current tissue state, and performance demands.
For this athlete, the story wasn’t just about strength symmetry. It was about respecting the knee’s history, anticipating its vulnerabilities, and choosing an intervention — in this case, hyaluronic acid — that addressed the most immediate barrier to availability. The numbers gave us confidence to move forward, but the decision-making lived in the grey space between those numbers.
For a deeper dive into integrative approaches like this, listen to From Special Forces to Preventative Medicine ft. Dr. Jesse Greer on Finding Small Wins, where we discuss bridging the gap between data and decision-making.
Free Download
Watch More Like This
Read More Like This
Related Podcasts
References
Altman RD, Hackel J, Niazi F, Shaw P, Nicholls M. Efficacy and safety of repeated courses of hyaluronic acid injections for knee osteoarthritis: A systematic review. Semin Arthritis Rheum. 2018;48(2):168-175. doi:10.1016/j.semarthrit.2018.01.009
Wang, A., Zhang, Q., Wang, N., Yu, C., Liu, R., Luo, Y., Zhao, Y., & Xiao, J. (2020). Cocktail of Hyaluronic Acid and Human Amniotic Mesenchymal Cells Effectively Repairs Cartilage Injuries in Sodium Iodoacetate-Induced Osteoarthritis Rats. Frontiers in Bioengineering and Biotechnology, 8. https://doi.org/10.3389/fbioe.2020.00087.
Wong, K., Zhang, S., Wang, M., Ren, X., Afizah, H., Lai, R., Lim, S., Lee, E., Hui, J., & Toh, W. (2020). Intra-articular injections of mesenchymal stem cell exosomes and hyaluronic acid improve structural and mechanical properties of repaired cartilage in a rabbit model.. Arthroscopy : the journal of arthroscopic & related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. https://doi.org/10.1016/j.arthro.2020.03.031.
Whyte, G., Bizzoco, L., & Gobbi, A. (2024). One-Step Cartilage Repair of Full-Thickness Knee Chondral Lesions Using a Hyaluronic Acid–Based Scaffold Embedded With Bone Marrow Aspirate Concentrate: Long-term Outcomes After Mean Follow-up Duration of 14 Years. The American Journal of Sports Medicine, 52, 3561 – 3568. https://doi.org/10.1177/03635465241287524.





