“Swelling & inflammation are neither good or bad. In fact, they are necessary for healing. It is simply a matter of managing them appropriately to optimize injury recovery.”
Adam Loiacono
Inflammation: A Natural Healing Response
Inflammation often gets a bad reputation, but it is an essential part of the body’s natural healing process. After surgery, inflammation signals the body’s immune response to protect the injured area and initiate healing. While excessive or prolonged inflammation can hinder recovery, controlled inflammation is crucial for tissue repair.
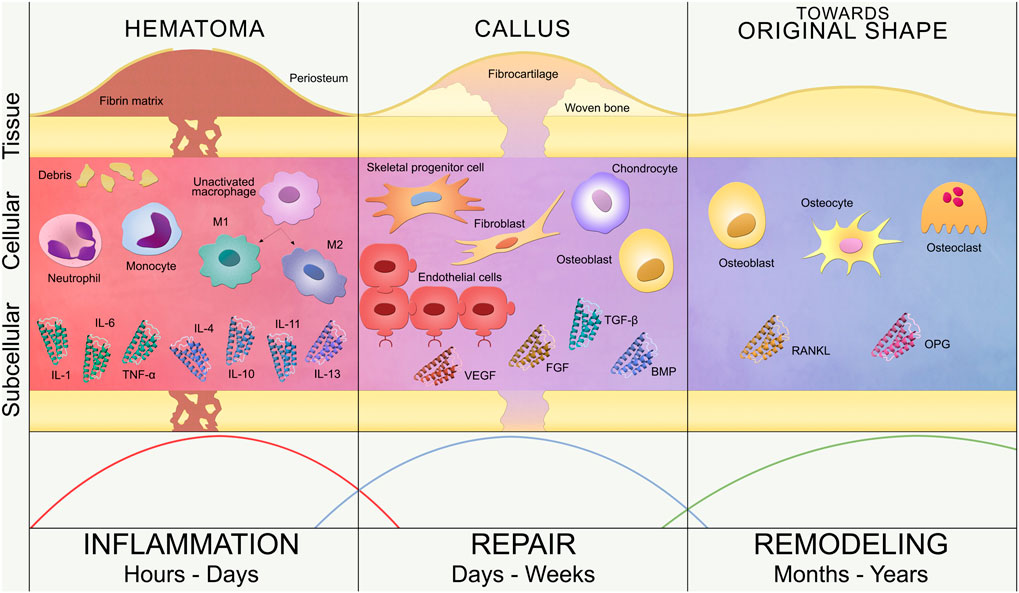
Understanding the Inflammatory Process
When tissue is damaged during injury or surgery, whether it’s muscle, tendon, or bone, the body responds by increasing blood flow to the area. This increased circulation brings immune cells such as macrophages, neutrophils, and cytokines to clean up debris and signal the need for tissue repair. The resulting swelling, redness, heat, and pain are common indicators of this response.
The inflammatory phase is highly variable depending on the tissue type, extent of the injury or surgery, and individual client factors such as age, immune function, overall health, etc. During this time, controlled management of inflammation is vital to prevent excessive swelling, maintain mobility, and set the foundation for tissue healing.
Benefits of Inflammation
Although inflammation can feel uncomfortable, it plays several important roles in healing:
- Debris Removal: Immune cells remove dead or damaged cells from the surgical site.
- Increased Circulation: Swelling brings nutrient-rich blood to the area to promote tissue repair.
- Growth Factor Activation: Inflammatory signals stimulate the release of growth factors, which aid in the repair of tissues such as tendons, ligaments, and bone.
Balancing Inflammation
Our goal is to support the body’s natural inflammatory process without allowing it to become excessive. I am not suggesting the use of non-steroidal anti-inflammatory drugs (NSAIDs, or commonly known as Advil or ibuprofen) are bad. I am suggesting us to consider the timing and use of these. There is evidence available to support how the use of NSAIDs delays healing and may slow recovery.
While we use modalities to manage swelling and pain, it’s essential to remember that complete elimination of inflammation is neither possible nor desirable. Instead, our approach should be to balance and control inflammation to optimize healing.
Acute Injury Swelling
Acute swelling, or edema, is a common response to injury and plays a significant role in increasing pain, reducing range of motion, and inhibiting muscle firing. Understanding the physiological processes behind swelling can help guide effective treatment strategies in the early stages of injury. At the cellular level, swelling is a critical component of the body’s acute inflammatory response, essential for initiating the healing process but often a source of discomfort and functional limitations.
pHysiological Processes
The acute inflammatory process increases blood flow to the injured area and transports several inflammatory mediators like histamines, cytokines, and prostaglandins. These mediators cause vasodilation and increased capillary permeability, allowing plasma proteins, white blood cells, and other healing factors to exit the bloodstream and enter the interstitial space. While this influx of cells and fluid helps with tissue repair and clearing debris, it also leads to localized swelling, or edema.
Swelling’s Impact on Pain
Swelling directly contributes to pain by increasing pressure within the tissue. As fluid accumulates, it raises extracellular pressure, compressing surrounding structures, including nerve endings. This compression sensitizes nociceptors, or pain receptors, sending signals to the brain that are interpreted as pain. Inflammatory mediators like bradykinin and prostaglandins further enhance this response by lowering the threshold for nociceptor activation, making the area more sensitive to stimuli. The resulting pain often limits voluntary movement, further contributing to functional impairment.
Reduction in Range of motion
Swelling can significantly reduce range of motion (ROM) by creating a physical barrier within the joint or surrounding soft tissues. The increased fluid volume in the extracellular space distends the tissues, making it difficult for muscles, tendons, and ligaments to move freely. Additionally, the increased pressure inside a swollen joint restricts its ability to move through its full range, often leading to stiffness. This reduction in ROM not only limits mobility but can also impair proper biomechanics, leading to compensatory movement patterns that increase the risk of further injury.

Example of a swollen lateral ankle from an ankle sprain.
Swelling Inhibits Muscles
Muscle activation is also inhibited by acute swelling. The accumulation of fluid and increased pressure within the tissues disrupts normal neuromuscular function, inhibiting the firing of muscles surrounding the injured area. This phenomenon, known as arthrogenic muscle inhibition (AMI), occurs when swelling and joint damage alter the sensory feedback from the joint to the central nervous system (CNS). As a result, motor control is disrupted, and muscles may become weak or unresponsive, limiting movement and stability around the joint.
The Lymphatic System & Swelling
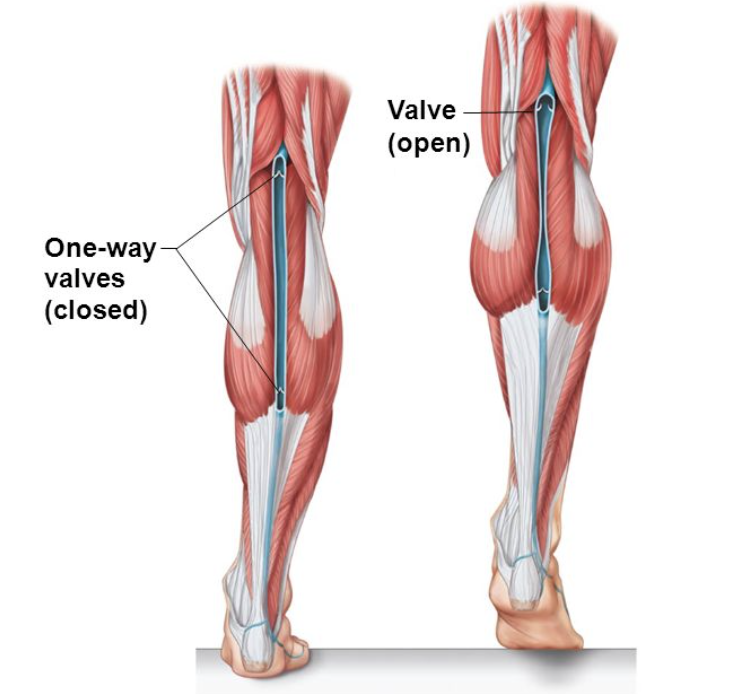
After an injury, there is an increase in hydrostatic pressure within the interstitial space due to fluid accumulation from damaged blood vessels. This rise in pressure pushes excess fluid, proteins, and waste into the lymphatic system. The lymphatic vessels, equipped with one-way valves, direct this fluid toward the heart, preventing backflow.
The increased pressure enhances lymphatic absorption, as fluid moves from areas of high pressure (injured tissue) to low pressure (lymphatic capillaries). This is part of Pascal’s Law. The one-way valves ensure unidirectional flow, maintaining efficient fluid drainage despite changes in pressure. This mechanism is crucial in reducing edema and promoting tissue recovery.
However, in the case of acute swelling after an injury, the system may become overwhelmed by the increased fluid load secondary to the changes in hydrostatic pressure. When the lymphatic system cannot keep up with the demand, fluid continues to accumulate, further exacerbating swelling. This creates a vicious cycle, where persistent swelling leads to prolonged pain, decreased mobility, and delayed muscle activation.
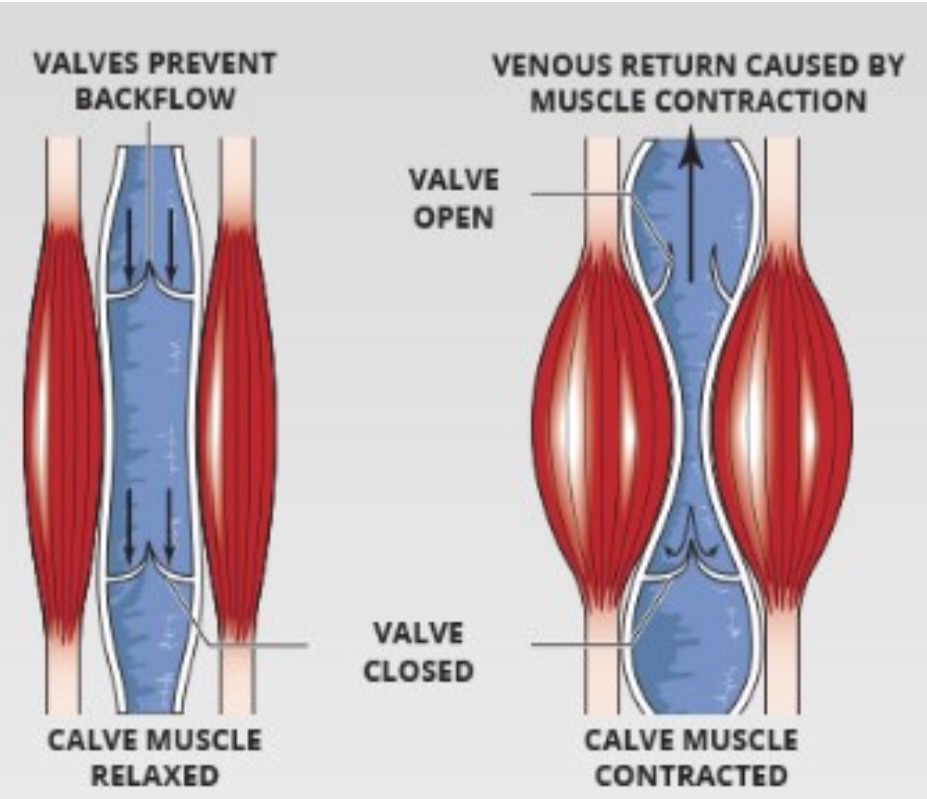
The lymphatic system is largely passive compared to the arterial system, which relies on the heart’s active pumping to circulate blood. Lymph fluid, however, lacks a central pump and instead depends on several passive mechanisms for movement. Key forces driving lymph flow include:
- External pressures, such as compression and muscle contractions, which compress lymph vessels and push fluid forward.
- Respiratory movements, where changes in thoracic pressure during breathing help propel lymph toward the central veins.
- Smooth muscle contractions within the walls of lymph vessels.
Together with the system’s one-way valves, these mechanisms guide lymph fluid toward the venous system for reabsorption.

Updating r.i.c.e. to p.e.a.c.e. & l.o.v.e.
Should we Ice?
Icing is commonly used for pain management in acute injuries due to its ability to numb the area and reduce pain by slowing neuronal conduction. However, its effectiveness in reducing swelling is debated.
Ice induces vasoconstriction, which reduces blood flow to the affected area, hindering the body’s natural healing process. By limiting circulation, ice also increase the viscosity of bodily fluids, making it harder for the lymphatic system to clear excess fluid. This process slows the removal of cellular debris, leading to prolonged swelling.
This interference with the body’s healing mechanisms may delay recovery by impeding the inflammatory phase necessary for tissue repair. Inflammation is crucial for clearing damaged cells and signaling tissue regeneration. Therefore, while ice can provide temporary pain relief, it may not be the optimal solution to manage swelling in the long term.
Active recovery approaches, which promote fluid movement and circulation, are increasingly recommended to facilitate better outcomes. By focusing on mechanical load, compression, and elevation, swelling can be more effectively managed without compromising tissue repair.
MODERN UPDATES
A more modern acronym that we can learn is PEACE and LOVE. The below graphic outlines several of the key components of this approach to help manage swelling and inflammation following an injury.

Compression for Swelling
The impact of Compression on Physiology
External compression increases hydrostatic pressure within tissues, counteracting some of the force that causes fluid to move out of the capillaries following tissue damage.
External pressure from compression modalities increases interstitial fluid pressure, promoting lymphatic fluid movement toward lymph vessels. The lymphatic system’s one-way valves ensure fluid flows in one direction, preventing back flow. Increased pressure enhances lymphatic return, helping reduce swelling by moving excess fluid from injured tissues toward the heart for reabsorption.
In the application of compression, or elevation, a “rebound phenomenon” or a “rebound effect” can result from the use of compression, or the transition from an elevated position to a dependent position. In elevation this can be attributed to the effects of gravity transitioning from an elevated position to a dependent position. In the case of improper application of pressure from external wraps, garments, or modalities, a tourniquet like effect is created that increases blood flow to the injured site following removal of the compression.
Static Compression: Wraps, Stockings, & Garments
Static compression refers to wraps, stockings, and compression garments that are worn continuously throughout the day. The benefit of static compression is long duration usage and low maintenance. The intention of using static compression is to provide enough external pressure to support the lymphatic system while natural movement throughout the day shuttles fluid into the lymph system’s one way valves.
Compression helps limit fluid accumulation in the injured area, reduces pain, and enhances lymphatic flow. By promoting proper circulation, it can prevent prolonged swelling and decrease recovery time. Additionally, compression provides mild support to the injured area, reducing excessive movement and promoting healing.
To be effective, compression wraps or tape should be applied with consistent, moderate pressure—enough to encourage fluid movement but not so tight that it impairs circulation. One essential principle is applying compression distal to proximal. Starting at the farthest point from the heart (e.g., the toes or fingers) and wrapping upward toward the heart helps guide the fluid in the correct direction through the lymphatic and venous systems. The pressure should gradually decrease as the wrap moves toward the proximal region, ensuring smooth fluid flow without creating a tourniquet effect.
Common errors in applying compression include:
- Excessive tightness: Overly tight wraps can impede blood flow and create ischemia, exacerbating swelling and causing discomfort.
- Inconsistent pressure: Uneven or loose wrapping may result in ineffective fluid movement, causing fluid to pool in the wrong areas.
- Skipping the distal-to-proximal approach: Incorrect direction of application can prevent proper drainage of swelling, potentially worsening the condition.
- Leaving compression on for too long: Prolonged compression without intermittent relief may result in skin irritation or impaired circulation.

The potential negative effect of static compression is improper gradients or improper application of pressure. Recall Pascal’s law, areas of fluid with high pressure move towards areas of low pressure. If external wraaps exert to much pressure, then as soon as that garment is removed a “rebound effect” can occur and an increase in swelling at the injured site can occur due to pressure gradients.
Specific garments like a JOBST full leg stocking are specifically created to have graduated pressure that supports movement of fluid distally to proximally to minimize any rebound effects. Several other socks with variable pressure exist to be able to accurately prescribe pressure based on limb size.


Dynamic Compression
Over the last 20 years the impact of technology has produced a wide variety of compression tools to assist with recovery in athletes. Two of the most popular brand name modalities are GameReady and NormaTec.
NormaTec and GameReady are passive modalities that use sequential compression to reduce swelling by inflating and deflating chambers around the limb. GameReady combines compression with cold therapy to enhance the modality and reduce pain.
The principles behind the two modalities of segmental external pressure supports the physiology of how the lymphatic system works. Athletes enjoy the use of both modalities from both an overall recovery and injury recovery perspectives. In terms of outcome measures following injury, there may be no additional benefit.
Clinically, the acute effects of short term reductions in pain and swelling can positively impact a rehab or therapy session. In the case of pain or swelling impeding progress in rehab or therapy, these potential short term pain and swelling changes allow therapists to provide other interventions such as exercise or manual therapy.



Movement & Muscle Contractions for Swelling
Muscle contractions are especially important for promoting lymphatic flow, as they compress surrounding tissues and lymphatic vessels, pushing fluid into the lymphatic capillaries and onward through larger lymphatic vessels.
When muscles contract, they apply pressure on lymphatic vessels. The one-way valves within these vessels prevent back flow, ensuring that fluid moves toward the heart. This process is crucial in reducing interstitial fluid that accumulates following injury, which leads to swelling (edema). Proper muscle contraction facilitates the removal of metabolic waste, proteins, and excess fluid from the injured site, speeding up tissue repair and reducing discomfort associated with swelling.
Devices like Marc Pro, Firefly, and Compex stimulate muscle contractions via electrical impulses delivered through electrodes placed on the skin. These contractions mimic the natural pumping action of the muscles, effectively pushing fluid into the lymphatic system, similar to how normal muscle movement works. However, these devices offer the advantage of creating controlled, gentle contractions without significantly loading the injured tissue, minimizing the risk of further injury and allowing for long duration treatments during periods of forced rest.
The MarcPro device is designed to generate non-fatiguing muscle contractions at a low frequency. The gentle contractions create a “pumping” effect, which encourages fluid movement into the lymphatic system. The low intensity of stimulation prevents muscle fatigue, allowing longer sessions without overworking the muscles, thereby enhancing recovery over time. This device is commonly used to facilitate post-exercise recovery and manage post-injury edema by continuously promoting lymphatic drainage.

The FireFly device works by stimulating the peroneal (fibular) nerve, located inferior to the fibular head, which in turn triggers muscle contractions in the lower leg. By targeting this specific nerve, the Firefly device enhances blood circulation and lymphatic flow in the lower limbs, an area particularly prone to swelling after injury or surgery. It is often used to prevent deep vein thrombosis (DVT) in surgical patients and promote faster recovery by improving fluid dynamics in the lower extremities. The Firefly unit has multiple intensity settings and can last up to 24 hours.


Compex units use electrical muscle stimulation (EMS) to stimulate various muscle groups, aiding in lymphatic flow. Similar to Marc Pro, Compex devices offer different stimulation programs, allowing for low-frequency contractions to improve circulation, reduce swelling, and flush out waste products. By activating the muscle pump mechanism, these devices help reduce edema while also improving recovery by increasing nutrient-rich blood flow to the affected area.


The muscle contractions induced by electrical stimulation create a rhythmic compressive force on tissues, facilitating fluid movement out of the swollen area. As fluid moves through the lymphatic vessels, it passes through lymph nodes, where waste products and excess proteins are filtered. The fluid is then returned to the bloodstream, where it is processed and removed from the body.
Electrical stimulation enhances this natural process by increasing the frequency and efficiency of muscle contractions, especially when the individual cannot engage in active movement due to pain or injury. The benefits of these devices lie in their ability to promote recovery without overloading the muscles or joints, making them ideal for managing swelling during both the acute and recovery phases of an injury.
While electrical stimulation devices are effective in reducing swelling, proper use is essential for optimal results. Placing electrodes incorrectly or using too high an intensity can lead to discomfort or even exacerbate swelling. Users should follow manufacturer guidelines and consult healthcare professionals to ensure appropriate settings and placement.
In conclusion, electrical stimulation devices like Marc Pro, Firefly, and Compex help manage swelling by enhancing the natural muscle pump.
Non-Painful Movement
Modified activity through non-impact exercises like biking or pool activities is a highly effective way to manage acute swelling following injury or surgery. These activities stimulate muscle contractions and circulation without placing undue stress on the injured tissues, promoting lymphatic drainage and reducing edema.
Stationary biking or light cycling offers a low-impact option to engage muscles, particularly in the lower body, without the high forces associated with weight-bearing activities like running. The rhythmic pedaling motion stimulates muscle contractions that activate the muscle pump mechanism, helping to move excess fluid out of the swollen area and into the lymphatic system. Biking encourages continuous blood flow and tissue oxygenation, which are essential for healing, while avoiding the mechanical impact that could exacerbate swelling.
The non-weight-bearing nature of biking also helps maintain range of motion in the injured limb without overloading it. This makes biking ideal for early-stage recovery, allowing for gentle reactivation of muscles and joints while aiding in the reduction of swelling.

Exercising in water provides a unique advantage for swelling management. The buoyancy of water significantly reduces the effective body weight, minimizing stress on injured tissues while still allowing for full-range motion. This reduction in body weight lowers joint impact, enabling more movement with less discomfort. Additionally, the hydrostatic pressure exerted by water naturally compresses the body, which can help push excess fluid back into the lymphatic and venous systems, promoting the reduction of swelling.
Pool activities, such as light swimming or water walking, combine the benefits of gentle movement with compression from hydrostatic pressure, making them an excellent intervention for managing acute swelling.

Take Home Points
- Acute Swelling and Inflammation: Swelling, or edema, occurs due to increased capillary permeability during the inflammatory response. This fluid accumulation increases pressure, causing pain, reduced range of motion, and inhibited muscle activation. Proper management, such as compression and elevation, is crucial for reducing swelling and promoting tissue recovery.
- Compression: External compression increases interstitial pressure, aiding lymphatic fluid movement and preventing fluid buildup. Techniques like static compression (garments, wraps) and dynamic compression (devices like GameReady) are effective. However, improper application can lead to rebound effects and exacerbate swelling.
- Movement and Electrical Stimulation: Non-impact exercises like biking or pool activities stimulate circulation and reduce edema. Electrical stimulation devices (e.g., Marc Pro, Firefly) create gentle muscle contractions, which help move fluid into the lymphatic system, improving lymphatic drainage and swelling reduction without stressing the injured area.
Progress Rehab with Expert Precision
After the swelling is gone, how to do progress rehab appropriately? Tune into episode 017 with Dr. Shireen Mansoori to learn how to progress with precision.

insightful videos
Subscribe today to Adam’s YouTube channel to get the latest on rehab, training, sports science, and so much more!




