“Posture isn’t good or bad—it just is.” – Dr. Jennifer Reiner-Marcello
What You Will Learn
- Posture is adaptation, not perfection, shaping performance across sports contexts.
- Movement should be judged by function and transfer, not visual aesthetics.
- Injury risk reduction demands individualized thresholds, not universal strength standards.
Introduction
For decades, posture has been painted in black and white terms: good vs. bad, military-straight vs. slouched and weak. In reality, posture and movement live in shades of gray. They are adaptive, fluid, and context-dependent. For athletes, posture is not a fixed “ideal” but a reflection of how the body organizes itself under gravity, load, and sport-specific demands.
In this episode of the Finding Small Wins Podcast, I welcome Dr. Jennifer Reiner-Marcello, founder of Stay in the Game and sports chiropractor with over 20 years of experience across MLB, collegiate athletics, and the private sector. Together, t challenge the myths of perfect posture, explore how structure influences performance, and explain why intervention in movement isn’t always the right call.
Whether you’re a physical therapist, performance coach, athletic trainer, or athlete, this episode provides a refreshing perspective: movement and posture are not problems to be fixed, but stories to be understood.
Jennifer’s Background
Dr. Jennifer Reiner-Marcello’s career spans collegiate athletics, professional baseball with the Padres and Twins, and private performance training for elite athletes. Her unique blend of strength and conditioning, sports medicine, and chiropractic care gives her a perspective few professionals can match.
At Stay in the Game, she provides high-level, customized programs for professional baseball players and rotational athletes. Her expertise lies in integrating manual therapy, movement assessment, and performance training into a seamless continuum. This multidisciplinary lens allows her to translate table-based insights directly into the weight room and onto the field—bridging the gap between healthcare and performance.
5 Episode Highlights
1. Posture as Adaptation
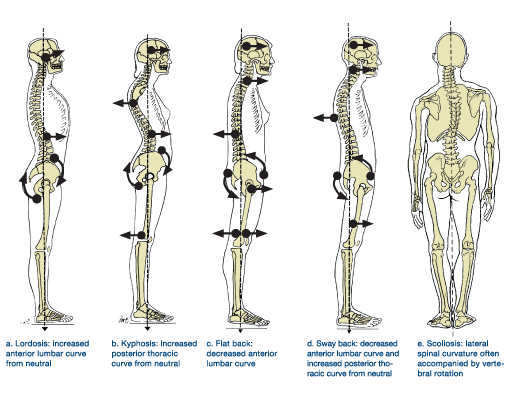
Traditional models often reduce posture to a binary: good versus bad, upright versus slouched, neutral versus dysfunctional. This framing has influenced everything from rehab textbooks to gym posters, creating a cultural obsession with “perfect” posture. Dr. Reiner-Marcello challenges this outdated lens, reminding us that posture is not a static snapshot to be judged, but a dynamic adaptation to the individual’s structure, sport demands, and environment.
“There’s no perfect posture—it’s simply how the body manages gravity and environment.”
For instance, consider the “cashew-shaped” torso of a swimmer or the forward head posture of a catcher. To an untrained eye, these might look pathological. Yet, in context, they serve as competitive advantages that allow the athlete to repeatedly perform their sport’s unique demands. The swimmer’s curve supports streamlined body position in water; the catcher’s crouch builds tolerance for hours behind the plate.
What matters most is not whether posture fits a textbook ideal, but whether it allows the athlete to perform, adapt, and stay healthy. Posture is simply the body’s way of negotiating gravity and environment at any given moment.
2. Movement IS Not Pretty vs. Ugly, Just Functional
In the same way posture has been mischaracterized, movement has long been judged aesthetically. Clean lines, symmetrical mechanics, and textbook form are often glorified, while deviations are labeled flawed. Dr. Reiner-Marcello pushes back on this idea, emphasizing that movement is not a beauty contest—it’s about function and effectiveness.
Take pitching as an example. A pitcher’s mechanics may appear awkward or inefficient on slow-motion video. Coaches might feel the urge to “clean it up.” But that same movement pattern may generate deception, improve timing, or create velocity in ways that give the pitcher an edge. Attempting to “fix” what looks ugly could strip away the very qualities that make the athlete effective.
“Movement just is—a reflection of what you have access to.”
Movement should therefore be assessed by whether it transfers to performance outcomes and supports tissue resilience, not whether it pleases the eye. What seems unconventional might actually be the key to long-term durability or competitive success.
3. When to Intervene (and When Not To)
Clinicians and coaches are trained to solve problems, and that bias often leads to intervening even when it isn’t necessary. Dr. Reiner-Marcello highlights the importance of clinical restraint: knowing when to let an asymmetry or imperfection remain untouched.
Many athletes thrive in what might appear to be dysfunction on the table. A pitcher with limited hip internal rotation might compensate with trunk mechanics that still allow for elite performance. Intervening to “correct” that hip restriction could unravel a finely tuned system that works for that athlete’s unique build and style.
“The hardest question is: should I intervene at all?”
Of course, there are times when intervention is essential—chronic pain, recurring breakdowns, or loss of availability signal a need for change. But the art lies in discernment: resisting the urge to chase every imperfection and instead focusing on whether the movement pattern is truly limiting performance or increasing injury risk.
4. Tools of the Trade: Manual, Stretching, and Exercise
Too often, manual therapy, stretching, and exercise are treated as competing camps within sports medicine. Dr. Reiner-Marcello reframes them as complementary tools along a continuum of adaptation.
Manual therapy creates awareness. It changes sensory input, reduces protective tone, and primes tissues for new motor patterns. Stretching reinforces range and introduces load at end ranges. Exercise, especially under resistance, engrains these changes in a durable, functional way. Finally, training contextualizes them under the stress of sport.
“Manual therapy primes the canvas; exercise paints the movement.”
In her view, the value is not in arguing which tool is best, but in sequencing them so that each step supports the next. When done correctly, athletes leave not just feeling better on the table, but capable of carrying those changes into the weight room and onto the field.
5. Injury Risk Reduction: No One-Size-Fits-All
The performance and rehab worlds love standards: a squat-to-bodyweight ratio, hamstring-to-quad strength percentages, or symmetry thresholds. While useful as rough guides, Dr. Reiner-Marcello warns against over-reliance on universal numbers. Athletes are not spreadsheets—they are archetypes with unique structures, strengths, and strategies.
“How strong is strong enough depends entirely on the athlete in front of you.”
For example, athletes with wide pelvises often display different loading strategies than those with narrow pelvises. Elastic athletes may rely more on tendon recoil, while force-dominant athletes generate performance through raw strength. Their injury risks and protective strategies are not the same.
Instead of chasing generic benchmarks, providers must ask: “What is strong enough for this athlete, in this role, in this sport?” A rotational athlete may need more mobility and elastic qualities; a lineman may require higher absolute force. Context dictates thresholds, not arbitrary standards.
Conclusion
Dr. Jennifer Reiner-Marcello reminds us that posture and movement are not puzzles to be solved but stories to be read. Perfect posture doesn’t exist, and chasing it can do more harm than good. Instead, success lies in understanding an athlete’s archetype, sport demands, and unique adaptations.
For providers, the message is clear: context matters more than conformity. For athletes, it’s a relief: your posture isn’t broken. It’s simply the way your body expresses performance.
- Stop labeling posture as “good” or “bad”—view it as adaptation.
- Movement quality should be judged by function and transfer, not aesthetics.
- Sometimes the best intervention is no intervention.
- Pair manual work with exercise for lasting change.
- Risk reduction strategies must fit the athlete’s structure and sport.
Episode Timeline
- 00:00 – Career Background – From gymnastics to MLB, Padres to Twins.
- 06:00 – Evolution in Pro Baseball – From taboo training rooms to proactive recovery.
- 12:00 – Defining Posture – From chiropractic school skepticism to posture as adaptation.
- 16:00 – Movement “Just Is” – Functional vs. aesthetic judgments.
- 20:00 – When to Intervene – The ethics of fixing vs. leaving.
- 27:00 – Manual Therapy & Exercise – Tools working in continuum.
- 34:00 – Injury Risk Frameworks – Strength, conditioning, symmetry—contextualized.
- 45:00 – Archetypes in Action – Narrow vs. wide athletes and programming choices.
- 53:00 – Models and Inflection Points – DNS, PRI, SFMA, and finding what works.
- 59:00 – Advice for Providers & Athletes – Curiosity, continuous learning, and finding complete programs.
Listen to the Full Episode Here






